Hospital

An intensive care unit (ICU) from a modern hospital

The Uniklinikum Aachen in Germany is the largest hospital in the world, count in a single building, with over 1200 beds.

All India Institute of Medical Sciences in Delhi, India
| Public infrastructure |
|---|
 Grand Coulee Dam |
Assets and facilities |
|
Concepts |
|
Issues and ideas |
|
Fields of study |
|
Examples
|
|
A hospital is a health care institution providing patient treatment with specialized medical and nursing staff and medical equipment.[1] The best-known type of hospital is the general hospital, which typically has an emergency department to treat urgent health problems ranging from fire and accident victims to a heart attack. A district hospital typically is the major health care facility in its region, with a large number of beds for intensive care and additional beds for patients who need long-term care. Specialized hospitals include trauma centers, rehabilitation hospitals, children's hospitals, seniors' (geriatric) hospitals, and hospitals for dealing with specific medical needs such as psychiatric treatment (see psychiatric hospital) and certain disease categories. Specialized hospitals can help reduce health care costs compared to general hospitals.[2] Hospitals are classified as general, specialty, or government depending on the sources of income received.
A teaching hospital combines assistance to people with teaching to medical students and nurses. The medical facility smaller than a hospital is generally called a clinic. Hospitals have a range of departments (e.g. surgery and urgent care) and specialist units such as cardiology. Some hospitals have outpatient departments and some have chronic treatment units. Common support units include a pharmacy, pathology, and radiology.
Hospitals are usually funded by the public sector, health organisations (for profit or nonprofit), health insurance companies, or charities, including direct charitable donations. Historically, hospitals were often founded and funded by religious orders, or by charitable individuals and leaders.[3]
Currently, hospitals are largely staffed by professional physicians, surgeons, nurses, and allied health practitioners, whereas in the past, this work was usually performed by the members of founding religious orders or by volunteers. However, there are various Catholic religious orders, such as the Alexians and the Bon Secours Sisters that still focus on hospital ministry in the late 1990s, as well as several other Christian denominations, including the Methodists and Lutherans, which run hospitals.[4] In accordance with the original meaning of the word, hospitals were originally "places of hospitality", and this meaning is still preserved in the names of some institutions such as the Royal Hospital Chelsea, established in 1681 as a retirement and nursing home for veteran soldiers.
.mw-parser-output .toclimit-2 .toclevel-1 ul,.mw-parser-output .toclimit-3 .toclevel-2 ul,.mw-parser-output .toclimit-4 .toclevel-3 ul,.mw-parser-output .toclimit-5 .toclevel-4 ul,.mw-parser-output .toclimit-6 .toclevel-5 ul,.mw-parser-output .toclimit-7 .toclevel-6 uldisplay:none
Contents
1 Etymology
2 Types
2.1 General & Acute Care
2.2 District
2.3 Specialised
2.4 Teaching
2.5 Clinics
3 Departments or wards
4 History
4.1 Early examples
4.2 Medieval Islamic world
4.3 Early modern and Enlightenment Europe
4.4 19th century
4.5 20th century and beyond
5 Funding
6 Buildings
6.1 Architecture
7 See also
8 References
9 Bibliography
9.1 History of hospitals
10 External links
Etymology

During peacetime, hospitals can be indicated by a variety of symbols. For example, a white 'H' on a blue background is often used in the United States. During times of armed conflict, a hospital may be marked with the emblem of the red cross, red crescent or red crystal in accordance with the Geneva Conventions.
| Look up hospital in Wiktionary, the free dictionary. |
During the Middle Ages, hospitals served different functions from modern institutions. Middle Ages hospitals were almshouses for the poor, hostels for pilgrims, or hospital schools. The word "hospital" comes from the Latin hospes, signifying a stranger or foreigner, hence a guest. Another noun derived from this, hospitium came to signify hospitality, that is the relation between guest and shelterer, hospitality, friendliness, and hospitable reception. By metonymy the Latin word then came to mean a guest-chamber, guest's lodging, an inn.[5]Hospes is thus the root for the English words host (where the p was dropped for convenience of pronunciation) hospitality, hospice, hostel and hotel. The latter modern word derives from Latin via the ancient French romance word hostel, which developed a silent s, which letter was eventually removed from the word, the loss of which is signified by a circumflex in the modern French word hôtel. The German word 'Spital' shares similar roots.
The grammar of the word differs slightly depending on the dialect. In the United States, hospital usually requires an article; in the United Kingdom and elsewhere, the word normally is used without an article when it is the object of a preposition and when referring to a patient ("in/to the hospital" vs. "in/to hospital"); in Canada, both uses are found.[citation needed]
Types

Lehigh Valley Hospital in Allentown, Pennsylvania
Some patients go to a hospital just for diagnosis, treatment, or therapy and then leave ("outpatients") without staying overnight; while others are "admitted" and stay overnight or for several days or weeks or months ("inpatients"). Hospitals usually are distinguished from other types of medical facilities by their ability to admit and care for inpatients whilst the others, which are smaller, are often described as clinics.
General & Acute Care
The best-known type of hospital is the general hospital, also known as an acute-care hospital. These facilities handle many kinds of disease and injury, and normally have an emergency department (sometimes known as "accident & emergency") or trauma center to deal with immediate and urgent threats to health. Larger cities may have several hospitals of varying sizes and facilities. Some hospitals, especially in the United States and Canada, have their own ambulance service.
District
A district hospital typically is the major health care facility in its region, with large numbers of beds for intensive care, critical care, and long-term care.
In California, "district hospital" refers specifically to a class of healthcare facility created shortly after World War II to address a shortage of hospital beds in many local communities.[6][7] Even today, district hospitals are the sole public hospitals in 19 of California's counties,[6] and are the sole locally-accessible hospital within 9 additional counties in which one or more other hospitals are present at substantial distance from a local community.[6] Twenty-eight of California's rural hospitals and 20 of its critical-access hospitals are district hospitals.[7] They are formed by local municipalities, have boards that are individually elected by their local communities, and exist to serve local needs.[6][7] They are a particularly important provider of healthcare to uninsured patients and patients with Medi-Cal (which is California's Medicaid program, serving low-income persons, some senior citizens, persons with disabilities, children in foster care, and pregnant women).[6][7] In 2012, District hospitals provided $54 million in uncompensated care in California.[7]
Specialised

Starship Children's Health is a children's hospital in Auckland, New Zealand.
Types of specialised hospitals include rehabilitation hospitals, children's hospitals, seniors' (geriatric) hospitals, long-term acute care facilities and hospitals for dealing with specific medical needs such as psychiatric problems (see psychiatric hospital), certain disease categories such as cardiac, oncology, or orthopedic problems, and so forth. In Germany specialised hospitals are called Fachkrankenhaus; an example is Fachkrankenhaus Coswig (thoracic surgery).
A hospital may be a single building or a number of buildings on a campus. Many hospitals with pre-twentieth-century origins began as one building and evolved into campuses. Some hospitals are affiliated with universities for medical research and the training of medical personnel such as physicians and nurses, often called teaching hospitals. Worldwide, most hospitals are run on a nonprofit basis by governments or charities. There are however a few exceptions, e.g. China, where government funding only constitutes 10% of income of hospitals. (need citation here. Chinese sources seem conflicted about the for-profit/non-profit ratio of hospitals in China)
Specialised hospitals can help reduce health care costs compared to general hospitals. For example, Narayana Health's Bangalore cardiac unit, which is specialised in cardiac surgery, allows for significantly greater number of patients. It has 3000 beds (more than 20 times the average American hospital) and in pediatric heart surgery alone, it performs 3000 heart operations annually, making it by far the largest such facility in the world.[8][2] Surgeons are paid on a fixed salary instead of per operation; thus, the costs to the hospital drops when the number of procedures increases, taking advantage of economies of scale.[8] Additionally, it is argued that costs go down as all its specialists become efficient by working on one "production line" procedure.[2]
Teaching

McMaster University Medical Centre is a teaching hospital in Hamilton, Ontario
A teaching hospital combines assistance to people with teaching to medical students and nurses and often is linked to a medical school, nursing school or university.
In some countries like UK exists the clinical attachment system that is defined as a period of time when a doctor is attached to a named supervisor in a clinical unit, with the broad aims of observing clinical practice in the UK and the role of doctors and other healthcare professionals in the National Health Service (NHS).
Clinics
The medical facility smaller than a hospital is generally called a clinic, and often is run by a government agency for health services or a private partnership of physicians (in nations where private practise is allowed). Clinics generally provide only outpatient services.
Departments or wards

Resuscitation room bed after a trauma intervention, showing the highly technical equipment of modern hospitals
Hospitals consist of departments, traditionally called wards, especially when they have beds for inpatients, when they are sometimes also called inpatient wards. Hospitals may have acute services such as an emergency department or specialist trauma centre, burn unit, surgery, or urgent care. These may then be backed up by more specialist units such as the following:
- Emergency department
- Cardiology
Intensive care unit- Paediatric intensive care unit
- Neonatal intensive care unit
- Cardiovascular intensive care unit
- Neurology
- Oncology
Obstetrics and gynaecology, colloquially, maternity ward
In addition, there is the department of nursing, often headed by a chief nursing officer or director of nursing. This department is responsible for the administration of professional nursing practice, research, and policy for the hospital. Nursing permeates every part of a hospital. Many units or wards have both a nursing and a medical director that serve as administrators for their respective disciplines within that specialty. For example, in an intensive care nursery, the director of neonatology is responsible for the medical staff and medical care while the nursing manager/director for the intensive care nursery is responsible for all of the nurses and nursing care in that unit/ward.
Some hospitals have outpatient departments and some have chronic treatment units such as behavioral health services, dentistry, dermatology, psychiatric ward, rehabilitation services, and physical therapy.
Common support units include a dispensary or pharmacy, pathology, and radiology. On the non-medical side, there often are medical records departments, release of information departments, information management (a.k.a. IM, IT or IS), clinical engineering (a.k.a. biomed), facilities management, plant ops (operations, also known as maintenance), dining services, and security departments.
History
Early examples

View of the Askleipion of Kos, the best preserved instance of an Asklepieion.
The earliest documented institutions aiming to provide cures were ancient Egyptian temples. In ancient Greece, temples dedicated to the healer-god Asclepius, known as Asclepieia functioned as centres of medical advice, prognosis, and healing.[9] In early India India, Fa Xian, a Chinese Buddhist monk who travelled across India c. CE 400, recorded examples of healing institutions.[10] According to the Mahavamsa, the ancient chronicle of Sinhalese royalty, written in the sixth century CE, King Pandukabhaya of Sri Lanka (r. 437–367 BCE) had lying-in-homes and hospitals (Sivikasotthi-Sala).[11] A hospital and medical training centre also existed at Gundeshapur, a major city in southwest of the Sassanid Persian Empire founded in CE 271 by Shapur I.[12]

Ruins of a two thousand years old hospital were discovered in the historical city of Anuradhapura Mihintale Sri Lanka

A physician taking the pulse of a patient. From a 17th-century copy of Avicenna's Canon of Medicine. Wellcome Library, London.
The declaration of Christianity as an accepted religion in the Roman Empire drove an expansion of the provision of care. Following the First Council of Nicaea in CE 325 construction of a hospital in every cathedral town was begun, including among the earliest hospitals by Saint Sampson in Constantinople and by Basil, bishop of Caesarea in modern-day Turkey.[13] By the twelfth century, Constantinople had two well-organised hospitals, staffed by doctors who were both male and female. Facilities included systematic treatment procedures and specialised wards for various diseases.[14]
Medieval Islamic world
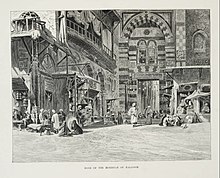
Entrance to the Qawaloon complex which housed the notable Qawaloon hospital.
The earliest general hospital was built in 805 in Baghdad by Harun Al-Rashid.[15][16] By the tenth century, Baghdad had five more hospitals, while Damascus had six hospitals by the 15th century and Córdoba alone had 50 major hospitals, many exclusively for the military.[17] Compared to contemporaneous Christian institutions, which were poor and sick relief facilities offered by some monasteries, The Islamic hospital was a more elaborate institution with a wider range of functions. In Islam, there was a moral imperative to treat the ill regardless of financial status. Islamic hospitals tended to be large, urban structures, and were largely secular institutions, many open to all, whether male or female, civilian or military, child or adult, rich or poor, Muslim or non-Muslim. The Islamic hospital served several purposes, as a center of medical treatment, a home for patients recovering from illness or accidents, an insane asylum, and a retirement home with basic maintenance needs for the aged and infirm.[18]
Hospitals in this era were the first to require medical diplomas to license doctors, and compensation for negligence could be made.[19]
Hospitals were forbidden by law to turn away patients who were unable to pay.[20] Eventually, charitable foundations called waqfs were formed to support hospitals, as well as schools.[20] Part of the state budget also went towards maintaining hospitals.[17]
Early modern and Enlightenment Europe
In Europe the medieval concept of Christian care evolved during the sixteenth and seventeenth centuries into a secular one. In England, after the dissolution of the monasteries in 1540 by King Henry VIII, the church abruptly ceased to be the supporter of hospitals, and only by direct petition from the citizens of London, were the hospitals St Bartholomew's, St Thomas's and St Mary of Bethlehem's (Bedlam) endowed directly by the crown; this was the first instance of secular support being provided for medical institutions.

A hospital ward in sixteenth century France.

1820 Engraving of Guy's Hospital in London one of the first voluntary hospitals to be established in 1724.
The voluntary hospital movement began in the early 18th century, with hospitals being founded in London by the 1720s, including Westminster Hospital (1719) promoted by the private bank C. Hoare & Co and Guy's Hospital (1724) funded from the bequest of the wealthy merchant, Thomas Guy.
Other hospitals sprang up in London and other British cities over the century, many paid for by private subscriptions. St Bartholomew's opened in London in 1730, and the London Hospital in 1752.
These hospitals represented a turning point in the function of the institution; they began to evolve from being basic places of care for the sick to becoming centres of medical innovation and discovery and the principal place for the education and training of prospective practitioners. Some of the era's greatest surgeons and doctors worked and passed on their knowledge at the hospitals.[21] They also changed from being mere homes of refuge to being complex institutions for the provision of medicine and care for sick. The Charité was founded in Berlin in 1710 by King Frederick I of Prussia as a response to an outbreak of plague.
The concept of voluntary hospitals also spread to Colonial America; the Bellevue Hospital Center opened in 1736; the Pennsylvania Hospital opened in 1752, New York Hospital in 1771, and Massachusetts General Hospital in 1811. When the Vienna General Hospital opened in 1784 (instantly becoming the world's largest hospital), physicians acquired a new facility that gradually developed into one of the most important research centres.[22]
Another Enlightenment era charitable innovation was the dispensary; these would issue the poor with medicines free of charge. The London Dispensary opened its doors in 1696 as the first such clinic in the British Empire. The idea was slow to catch on until the 1770s, when many such organisations began to appear, including the Public Dispensary of Edinburgh (1776), the Metropolitan Dispensary and Charitable Fund (1779) and the Finsbury Dispensary (1780). Dispensaries were also opened in New York 1771, Philadelphia 1786, and Boston 1796.[23]
The Royal Naval Hospital, Stonehouse, Plymouth, was a pioneer of hospital design in having "pavilions" to minimize the spread of infection. John Wesley visited in 1785, and commented "I never saw anything of the kind so complete; every part is so convenient, and so admirably neat. But there is nothing superfluous, and nothing purely ornamented, either within or without." This revolutionary design was made more widely known by John Howard, the philanthropist. In 1787 the French government sent two scholar administrators, Coulomb and Tenon, who had visited most of the hospitals in Europe.[24] They were impressed and the "pavilion" design was copied in France and throughout Europe.
19th century

A ward of the hospital at Scutari where Florence Nightingale worked and helped to restructure the modern hospital
English physician Thomas Percival (1740–1804) wrote a comprehensive system of medical conduct, Medical Ethics; or, a Code of Institutes and Precepts, Adapted to the Professional Conduct of Physicians and Surgeons (1803) that set the standard for many textbooks.[25] In the mid-19th century, hospitals and the medical profession became more professionalised, with a reorganisation of hospital management along more bureaucratic and administrative lines. The Apothecaries Act 1815 made it compulsory for medical students to practise for at least half a year at a hospital as part of their training.[26]
Florence Nightingale pioneered the modern profession of nursing during the Crimean War when she set an example of compassion, commitment to patient care and diligent and thoughtful hospital administration. The first official nurses' training programme, the Nightingale School for Nurses, was opened in 1860, with the mission of training nurses to work in hospitals, to work with the poor and to teach.[27] Nightingale was instrumental in reforming the nature of the hospital, by improving sanitation standards and changing the image of the hospital from a place the sick would go to die, to an institution devoted to recuperation and healing. She also emphasised the importance of statistical measurement for determining the success rate of a given intervention and pushed for administrative reform at hospitals.[28]
By the late 19th century, the modern hospital was beginning to take shape with a proliferation of a variety of public and private hospital systems. By the 1870s, hospitals had more than trebled their original average intake of 3,000 patients. In continental Europe the new hospitals generally were built and run from public funds. The National Health Service, the principal provider of health care in the United Kingdom, was founded in 1948. During the nineteenth century, the Second Viennese Medical School emerged with the contributions of physicians such as Carl Freiherr von Rokitansky, Josef Škoda, Ferdinand Ritter von Hebra, and Ignaz Philipp Semmelweis. Basic medical science expanded and specialisation advanced. Furthermore, the first dermatology, eye, as well as ear, nose, and throat clinics in the world were founded in Vienna, being considered as the birth of specialised medicine.[29]
20th century and beyond
By the late 19th and the beginning 20th century, medical advancements such as anesthesia and sterile techniques that could make surgery less risky, and availability of more advanced diagnostic devices such as X-rays continued to make hospitals a more attractive option for treatment. The number of hospitalizations in the United States continued to grow and reached its peak in 1981 with 171 admissions per 1000 Americans and 6933 hospitals.[30]
This trend, however, has been reversed since then, with the rate of hospitalization falling by more than 10% and the number of US hospitals shrinking from 6933 in 1981 to 5534 in 2016.[31] Among the reasons for this are the increasing availability of more complex care elsewhere such as at home or at the physicians' offices and also the less therapeutic and more life-threatening image of the hospitals in the eyes of the public.[32][30]
Microhospitals, which range from eight beds to fifty, are expanding in the United States.[33]
Modern hospitals measure various efficiency metrics such as occupancy rates, average length of stay, time to service, patient satisfaction, physician performance, patient readmission rate, inpatient mortality rate, and case mix index.[34]
Modern hospitals are in part defined by their ability to admit patients into inpatient care, which affects reimbursement. In the US, a patient may sleep in a hospital bed, but considered outpatient and "under observation" if not formally admitted.[35] In the US, inpatient stays are covered under Medicare Part A, but a hospital might keep a patient under observation which is only covered under Medicare Part B, and subjects the patient to additional coinsurance costs.[35]
In the United States, occupancy rates dropped from 77% in 1980 to 60% in 2013.[36] US hospital-based healthcare systems reported poor financial results in 2016 and 2017 as they adapted to healthcare reform and continued decline in admissions.[37] Hospitals were also affected by the Center for Medicare and Medicaid Services (CMS) rules, including in 2013 included a controversial "two-midnight" rule for inpatient admissions.[38] The rule was intended to reduce long-term "observation" stays, which increased from 3% to 8% of all cases between 2006 and 2011.[35]
Funding

Clinical Hospital Dubrava in Zagreb, Croatia
Modern hospitals are either funded by the government of the country in which they are situated, or survive financially by competing in the private sector (a number of hospitals also are still supported by the historical type of charitable or religious associations).
In the United Kingdom for example, a relatively comprehensive, "free at the point of delivery" health care system exists, funded by the state. Hospital care is thus relatively easily available to all legal residents, although free emergency care is available to anyone, regardless of nationality or status. As hospitals prioritise their limited resources, there is a tendency for 'waiting lists' for non-crucial treatment in countries with such systems, as opposed to letting higher-payers get treated first, so sometimes those who can afford it take out private health care to get treatment more quickly.[39]
In some countries such as the USA, hospitals typically operate privately and in some cases on a for-profit basis; for example, the multinational corporation Hospital Corporation of America operates hospitals across the country.[40] The list of procedures and their prices is called a chargemaster; however, these prices don't reflect the typical cost of the procedure, which is typically lower due to in-network negotiation.[41]
Where for-profit hospitals in such countries admit uninsured patients in emergency situations (such as during and after Hurricane Katrina in the USA), they incur direct financial losses,[40] ensuring that there is a clear disincentive to admit such patients. In the United States, laws exist to ensure patients receive care in life-threatening emergency situations regardless of the patient's ability to pay.[42]
As the quality of health care has increasingly become an issue around the world, hospitals have increasingly had to pay serious attention to this matter. Independent external assessment of quality is one of the most powerful ways to assess this aspect of health care, and hospital accreditation is one means by which this is achieved. In many parts of the world such accreditation is sourced from other countries, a phenomenon known as international healthcare accreditation, by groups such as Accreditation Canada from Canada, the Joint Commission from the USA, the Trent Accreditation Scheme from Great Britain, and Haute Authorité de santé (HAS) from France.
Buildings

The medical center at the University of Virginia shows the growing trend for modern architecture in hospitals.
Architecture

The National Health Service Norfolk and Norwich University Hospital in the UK, showing the utilitarian architecture of many modern hospitals

Hospital chapel at Fawcett Memorial Hospital (Port Charlotte, Florida)
Modern hospital buildings are designed to minimise the effort of medical personnel and the possibility of contamination while maximising the efficiency of the whole system. Travel time for personnel within the hospital and the transportation of patients between units is facilitated and minimised. The building also should be built to accommodate heavy departments such as radiology and operating rooms while space for special wiring, plumbing, and waste disposal must be allowed for in the design.[43]
However, many hospitals, even those considered "modern", are the product of continual and often badly managed growth over decades or even centuries, with utilitarian new sections added on as needs and finances dictate. As a result, Dutch architectural historian Cor Wagenaar has called many hospitals:
- "... built catastrophes, anonymous institutional complexes run by vast bureaucracies, and totally unfit for the purpose they have been designed for ... They are hardly ever functional, and instead of making patients feel at home, they produce stress and anxiety."[44]
Some newer hospitals now try to re-establish design that takes the patient's psychological needs into account, such as providing more fresh air, better views and more pleasant colour schemes. These ideas harken back to the late eighteenth century, when the concept of providing fresh air and access to the 'healing powers of nature' were first employed by hospital architects in improving their buildings.[44]
The research of British Medical Association is showing that good hospital design can reduce patient's recovery time. Exposure to daylight is effective in reducing depression. Single-sex accommodation help ensure that patients are treated in privacy and with dignity. Exposure to nature and hospital gardens is also important – looking out windows improves patients' moods and reduces blood pressure and stress level. Open windows in patient rooms have also demonstrated some evidence of beneficial outcomes by improving airflow and increased microbial diversity.[45][46] Eliminating long corridors can reduce nurses' fatigue and stress.[47]
Another ongoing major development is the change from a ward-based system (where patients are accommodated in communal rooms, separated by movable partitions) to one in which they are accommodated in individual rooms. The ward-based system has been described as very efficient, especially for the medical staff, but is considered to be more stressful for patients and detrimental to their privacy. A major constraint on providing all patients with their own rooms is however found in the higher cost of building and operating such a hospital; this causes some hospitals to charge for private rooms.[48]
See also
- History of medicine
- Lists of hospitals
- Burn center
- Hospital information system
- Trauma center
- The Waiting Room
- Walk-in clinic
References
^ "Hospitals". World Health Organization. Retrieved 2018-01-24..mw-parser-output cite.citationfont-style:inherit.mw-parser-output qquotes:"""""""'""'".mw-parser-output code.cs1-codecolor:inherit;background:inherit;border:inherit;padding:inherit.mw-parser-output .cs1-lock-free abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-lock-limited a,.mw-parser-output .cs1-lock-registration abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-lock-subscription abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registrationcolor:#555.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration spanborder-bottom:1px dotted;cursor:help.mw-parser-output .cs1-hidden-errordisplay:none;font-size:100%.mw-parser-output .cs1-visible-errorfont-size:100%.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-formatfont-size:95%.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-leftpadding-left:0.2em.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-rightpadding-right:0.2em
^ abc "India's 'production line' heart hospital". bbcnews.com. 1 August 2010. Retrieved 13 October 2013.
^ Hall, Daniel (December 2008). "Altar and Table: A phenomenology of the surgeon-priest". Yale Journal of Biology and Medicine. 81 (4): 193–98. PMC 2605310. PMID 19099050.Although physicians were available in varying capacities in ancient Rome and Athens, the institution of a hospital dedicated to the care of the sick was a distinctly Christian innovation rooted in the monastic virtue and practise of hospitality. Arranged around the monastery were concentric rings of buildings in which the life and work of the monastic community was ordered. The outer ring of buildings served as a hostel in which travellers were received and boarded. The inner ring served as a place where the monastic community could care for the sick, the poor and the infirm. Monks were frequently familiar with the medicine available at that time, growing medicinal plants on the monastery grounds and applying remedies as indicated. As such, many of the practicing physicians of the Middle Ages were also clergy.
^ Lovoll, Odd (1998). A Portrait of Norwegian Americans Today. U of Minnesota Press. p. 192. ISBN 978-0816628322.
^ Cassell's Latin Dictionary, revised by J. Marchant & J. Charles, 260th. thousand.
^ abcde "Our Background". District Hospital Leadership Forum. Retrieved 10 July 2014.
^ abcde Knox, Dennis. "District Hospitals' Important Mission". Payers &–° Providers. Retrieved 10 July 2014.
^ ab "Narayana Hrudayalaya Hospitals". fastcompany.com. 7 February 2012. Archived from the original on 3 October 2013. Retrieved 13 October 2013.
^ Risse, G.B. Mending bodies, saving souls: a history of hospitals. 1990. p. 56
^ Legge, James (1965). A Record of Buddhistic Kingdoms: Being an Account by the Chinese Monk Fâ-Hien of his Travels in India and Ceylon (CE 399–414) in Search of the Buddhist Books of Discipline.
[publisher missing][page needed]
^ Prof. Arjuna Aluvihare, "Rohal Kramaya Lovata Dhayadha Kale Sri Lankikayo" Vidhusara Science Magazine, November 1993.
^ The American Journal of Islamic Social Sciences 22:2 Mehmet Mahfuz Söylemez, The Gundeshapur School: Its History, Structure, and Functions, p. 3.
^ Catholic Encyclopedia – [1] (2009) Accessed April 2011.
^ Byzantine medicine
^ Husain F. Nagamia, [Islamic Medicine History and Current practise], (2003), p. 24.
^ Sir Glubb, John Bagot (1969), A Short History of the Arab Peoples, retrieved 25 January 2008
^ ab "The Islamic Roots of the Modern Hospital". aramcoworld.com. Retrieved 20 March 2017.
^ Islamic Culture and the Medical Arts: Hospitals, United States National Library of Medicine This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
^ Alatas, Syed Farid (2006). "From Jami'ah to University: Multiculturalism and Christian–Muslim Dialogue". Current Sociology. 54 (1): 112–32. doi:10.1177/0011392106058837.
^ ab
Rise and spread of Islam. Gale. 2002. p. 419. ISBN 978-0787645038.
^ Reinarz, Jonathan (2007). "Corpus Curricula: Medical Education and the Voluntary Hospital Movement". Brain, Mind and Medicine: Essays in Eighteenth-Century Neuroscience. pp. 43–52. doi:10.1007/978-0-387-70967-3_4. ISBN 978-0387709666.
^ Roderick E. McGrew, Encyclopedia of Medical History (Macmillan 1985), p. 139.
^ Michael Marks Davis; Andrew Robert Warner (1918). Dispensaries, Their Management and Development: A Book for Administrators, Public Health Workers, and All Interested in Better Medical Service for the People. MacMillan. pp. 2–3.
^ Surgeon Vice Admiral A Revell in http://www.histansoc.org.uk/uploads/9/5/5/2/9552670/volume_19.pdf
^ Waddington Ivan (1975). "The Development of Medical Ethics - A Sociological Analysis". Medical History. 19 (1): 36–51. doi:10.1017/s002572730001992x. PMC 1081608. PMID 1095851.
^ Porter, Roy (1999) [1997]. The Greatest Benefit to Mankind: A Medical History of Humanity from Antiquity to the Present. New York: W.W. Norton & Company. pp. 316–17. ISBN 978-0393319804.
^ Kathy Neeb (2006). Fundamentals of Mental Health Nursing. Philadelphia: F.A. Davis Company. ISBN 978-0803620346.
^ Nightingale, Florence (August 1999). Florence Nightingale: Measuring Hospital Care Outcomes. ISBN 978-0866885591. Retrieved 13 March 2010.
^ Erna Lesky, The Vienna Medical School of the 19th Century (Johns Hopkins University Press, 1976)
^ ab Emanuel, Ezekiel J. (2018-02-25). "Opinion | Are Hospitals Becoming Obsolete?". The New York Times.
^ "Fast Facts on U.S. Hospitals, 2018 | AHA".
^ https://www.cdc.gov/hai/pdfs/hai/infections_deaths.pdf
^ Staff. "5 common questions about micro-hospitals, answered". www.beckershospitalreview.com. Retrieved 2018-11-25.
^ "Hospital Industry's 10 Most Critical Metrics – Guiding Metrics". guidingmetrics.com. Retrieved 2018-11-25.
^ abc "Two-Midnight and Observation Rule — Chicago Medical Society". www.cmsdocs.org. Archived from the original on 2018-11-25. Retrieved 2018-11-25.
^ "As admissions have slumped and outpatient care booms, hospitals closing or shrinking". Modern Healthcare. Retrieved 2018-11-25.
^ "How U.S. Hospitals and Health Systems Can Reverse Their Sliding Financial Performance". Harvard Business Review. 2017-10-05. Retrieved 2018-11-25.
^ "CMS drops two-midnight rule's inpatient payment cuts". Modern Healthcare. Retrieved 2018-11-25.
^ Johnston, Martin (21 January 2008). "Surgery worries create insurance boom". The New Zealand Herald. Retrieved 3 October 2011.
^ ab Hospitals in New Orleans see surge in uninsured patients but not public funds – USA Today, Wednesday 26 April 2006
^ "Battling the Chargemaster: A Simple Remedy to Balance Billing for Unavoidable Out-of-Network Care". AJMC. Retrieved 2018-12-10.
^ "Emergency Medical Treatment & Labor Act (EMTALA)". centres for Medicare & Medicaid Services. 2012-03-26. Retrieved 17 May 2013.
^ Annmarie Adams, Medicine by Design: The Architect and the Modern Hospital, 1893–1943 (2009)
^ ab Healing by design Archived 17 October 2007 at the Wayback Machine. – Ode Magazine, July/August 2006 issue. Accessed 10 February 2008.
^ Sample, Ian (2012-02-20). "Open hospital windows to stem spread of infections, says microbiologist". The Guardian. Retrieved 2018-03-12.
^ Bowdler, Neil (2013-04-26). "Closed windows 'increase infection'". BBC News. Retrieved 2018-03-12.
^ "The psychological and social needs of patients". British Medical Association. 7 January 2011. Archived from the original on 14 March 2011. Retrieved 14 March 2011.
^ Health administrators go shopping for new hospital designs Archived 26 December 2008 at the Wayback Machine. – National Review of Medicine, Monday 15 November 2004, Volume 1 No. 21
Bibliography
History of hospitals
- Brockliss, Lawrence, and Colin Jones. "The Hospital in the Enlightenment," in The Medical World of Early Modern France (Oxford UP, 1997), pp. 671–729; covers France 1650–1800
- Chaney, Edward (2000),"'Philanthropy in Italy': English Observations on Italian Hospitals 1545–1789", in: The Evolution of the Grand Tour: Anglo-Italian Cultural Relations since the Renaissance, 2nd ed. London, Routledge, 2000. https://books.google.com/books/about/The_evolution_of_the_grand_tour.html?id=rYB_HYPsa8gC
- Connor, J.T.H. "Hospital History in Canada and the United States," Canadian Bulletin of Medical History, 1990, Vol. 7 Issue 1, pp. 93–104
- Crawford, D.S. Bibliography of Histories of Canadian hospitals and schools of nursing.
- Gorsky, Martin. "The British National Health Service 1948–2008: A Review of the Historiography," Social History of Medicine, December 2008, Vol. 21 Issue 3, pp. 437–60
- Harrison, Mar, et al. eds. From Western Medicine to Global Medicine: The Hospital Beyond the West (2008)
- Horden, Peregrine. Hospitals and Healing From Antiquity to the Later Middle Ages (2008)
- McGrew, Roderick E. Encyclopedia of Medical History (1985)
Morelon, Régis; Rashed, Roshdi (1996), Encyclopedia of the History of Arabic Science, 3, Routledge, ISBN 978-0415124102- Porter, Roy. The Hospital in History, with Lindsay Patricia Granshaw (1989)
ISBN 978-0415003759
Risse, Guenter B. Mending Bodies, Saving Souls: A History of Hospitals (1999); world coverage- Rosenberg, Charles E. The Care of Strangers: The Rise of America's Hospital System (1995); history to 1920
- Scheutz, Martin et al. eds. Hospitals and Institutional Care in Medieval and Early Modern Europe (2009)
- Wall, Barbra Mann. American Catholic Hospitals: A Century of Changing Markets and Missions (Rutgers University Press, 2011).
ISBN 978-0813549408
External links
| Wikimedia Commons has media related to Hospital. |
- Database
"Global and Multilanguage Database of public and private hospitals". hospitalsworldguide.com.
"Directory and Ranking of more than 17.000 Hospitals worldwide". hospitals.webometrics.info.
"Medical History". Open Access Scholarly Journal.