Cardiovascular disease
| Cardiovascular disease | |
|---|---|
 | |
Micrograph of a heart with fibrosis (yellow) and amyloidosis (brown). Movat's stain. | |
| Specialty | Cardiology |
| Usual onset | Older adults[1] |
| Types | Coronary artery diseases, stroke, heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy[2][3] |
| Prevention | Healthy eating, exercise, avoiding tobacco smoke, limited alcohol intake[2] |
| Treatment | Treating high blood pressure, high blood lipids, diabetes[2] |
| Deaths | 17.9 million / 32% (2015)[4] |
Cardiovascular disease (CVD) is a class of diseases that involve the heart or blood vessels.[2] Cardiovascular disease includes coronary artery diseases (CAD) such as angina and myocardial infarction (commonly known as a heart attack).[2] Other CVDs include stroke, heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy, heart arrhythmia, congenital heart disease, valvular heart disease, carditis, aortic aneurysms, peripheral artery disease, thromboembolic disease, and venous thrombosis.[2][3]
The underlying mechanisms vary depending on the disease.[2] Coronary artery disease, stroke, and peripheral artery disease involve atherosclerosis.[2] This may be caused by high blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol, poor diet, and excessive alcohol consumption, among others.[2] High blood pressure results in 13% of CVD deaths, while tobacco results in 9%, diabetes 6%, lack of exercise 6% and obesity 5%.[2] Rheumatic heart disease may follow untreated strep throat.[2]
It is estimated that 90% of CVD is preventable.[5] Prevention of atherosclerosis involves improving risk factors through: healthy eating, exercise, avoidance of tobacco smoke and limiting alcohol intake.[2] Treating risk factors, such as high blood pressure, blood lipids and diabetes is also beneficial.[2] Treating people who have strep throat with antibiotics can decrease the risk of rheumatic heart disease.[6] The use of aspirin in people, who are otherwise healthy, is of unclear benefit.[7][8]
Cardiovascular diseases are the leading cause of death globally.[2] This is true in all areas of the world except Africa.[2] Together they resulted in 17.9 million deaths (32.1%) in 2015, up from 12.3 million (25.8%) in 1990.[4][3]Deaths, at a given age, from CVD are more common and have been increasing in much of the developing world, while rates have declined in most of the developed world since the 1970s.[9][10] Coronary artery disease and stroke account for 80% of CVD deaths in males and 75% of CVD deaths in females.[2] Most cardiovascular disease affects older adults. In the United States 11% of people between 20 and 40 have CVD, while 37% between 40 and 60, 71% of people between 60 and 80, and 85% of people over 80 have CVD.[1] The average age of death from coronary artery disease in the developed world is around 80 while it is around 68 in the developing world.[9] Disease onset is typically seven to ten years earlier in men as compared to women.[11]
.mw-parser-output .toclimit-2 .toclevel-1 ul,.mw-parser-output .toclimit-3 .toclevel-2 ul,.mw-parser-output .toclimit-4 .toclevel-3 ul,.mw-parser-output .toclimit-5 .toclevel-4 ul,.mw-parser-output .toclimit-6 .toclevel-5 ul,.mw-parser-output .toclimit-7 .toclevel-6 uldisplay:none
Contents
1 Types
2 Risk factors
2.1 Genetics
2.2 Age
2.3 Sex
2.4 Tobacco
2.5 Physical inactivity
2.6 Diet
2.7 Sleep
2.8 Celiac disease
2.9 Socioeconomic disadvantage
2.10 Air pollution
2.11 Cardiovascular risk assessment
2.12 Occupational exposure
2.12.1 Non-chemical risk factors
2.12.2 Chemical risk factors
2.13 Somatic mutations
3 Pathophysiology
4 Screening
5 Prevention
5.1 Diet
5.2 Medication
5.3 Physical activity
5.4 Dietary supplements
6 Management
7 Epidemiology
8 Research
9 References
10 External links
Types

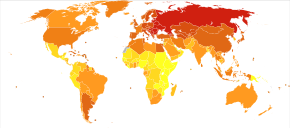
Disability-adjusted life year for inflammatory heart diseases per 100,000 inhabitants in 2004[12].mw-parser-output .refbeginfont-size:90%;margin-bottom:0.5em.mw-parser-output .refbegin-hanging-indents>ullist-style-type:none;margin-left:0.mw-parser-output .refbegin-hanging-indents>ul>li,.mw-parser-output .refbegin-hanging-indents>dl>ddmargin-left:0;padding-left:3.2em;text-indent:-3.2em;list-style:none.mw-parser-output .refbegin-100font-size:100%
no data
less than 70
70–140
140–210
210–280
280–350
350–420
420–490
490–560
560–630
630–700
700–770
more than 770
There are many cardiovascular diseases involving the blood vessels. They are known as vascular diseases.
Coronary artery disease (also known as coronary heart disease and ischemic heart disease)
Peripheral arterial disease – disease of blood vessels that supply blood to the arms and legs
Cerebrovascular disease – disease of blood vessels that supply blood to the brain (includes stroke)- Renal artery stenosis
- Aortic aneurysm
There are also many cardiovascular diseases that involve the heart.
Cardiomyopathy – diseases of cardiac muscle
Hypertensive heart disease – diseases of the heart secondary to high blood pressure or hypertension
Heart failure - a clinical syndrome caused by the inability of the heart to supply sufficient blood to the tissues to meet their metabolic requirements
Pulmonary heart disease – a failure at the right side of the heart with respiratory system involvement
Cardiac dysrhythmias – abnormalities of heart rhythm- Inflammatory heart disease
Endocarditis – inflammation of the inner layer of the heart, the endocardium. The structures most commonly involved are the heart valves.- Inflammatory cardiomegaly
Myocarditis – inflammation of the myocardium, the muscular part of the heart, caused most often by viral infection and less often by bacterial infections, certain medications, toxins, and autoimmune disorders. It is characterized in part by infiltration of the heart by lymphocyte and monocyte types of white blood cells.
Eosinophilic myocarditis - inflammation of the myocardium caused by pathologically activated eosinophilic white blood cells. This disorder differs from myocarditis in its causes and treatments.
- Valvular heart disease
Congenital heart disease – heart structure malformations existing at birth
Rheumatic heart disease – heart muscles and valves damage due to rheumatic fever caused by Streptococcus pyogenes a group A streptococcal infection.
Risk factors
There are many risk factors for heart diseases: age, gender, tobacco use, physical inactivity, excessive alcohol consumption, unhealthy diet, obesity, genetic predisposition and family history of cardiovascular disease, raised blood pressure (hypertension), raised blood sugar (diabetes mellitus), raised blood cholesterol (hyperlipidemia), undiagnosed celiac disease, psychosocial factors, poverty and low educational status, and air pollution.[13][14][15][16][17] While the individual contribution of each risk factor varies between different communities or ethnic groups the overall contribution of these risk factors is very consistent.[18] Some of these risk factors, such as age, gender or family history/genetic predisposition, are immutable; however, many important cardiovascular risk factors are modifiable by lifestyle change, social change, drug treatment (for example prevention of hypertension, hyperlipidemia, and diabetes).[19] People with obesity are at increased risk of atherosclerosis of the coronary arteries.[20]
Genetics
Genetic factors influence the development of cardiovascular disease in men who are less than 55 years-old and in women who are less than 65 years old.[19] Cardiovascular disease in a person's parents increases their risk by 3 fold.[21] Multiple single nucleotide polymorphisms (SNP) have been found to be associated with cardiovascular disease in genetic association studies,[22][23] but usually their individual influence is small, and genetic contributions to cardiovascular disease are poorly understood.[23]
Age

Calcified heart of an older woman with cardiomegaly
Age is the most important risk factor in developing cardiovascular or heart diseases, with approximately a tripling of risk with each decade of life.[24] Coronary fatty streaks can begin to form in adolescence.[25] It is estimated that 82 percent of people who die of coronary heart disease are 65 and older.[26] Simultaneously, the risk of stroke doubles every decade after age 55.[27]
Multiple explanations are proposed to explain why age increases the risk of cardiovascular/heart diseases. One of them relates to serum cholesterol level.[28] In most populations, the serum total cholesterol level increases as age increases. In men, this increase levels off around age 45 to 50 years. In women, the increase continues sharply until age 60 to 65 years.[28]
Aging is also associated with changes in the mechanical and structural properties of the vascular wall, which leads to the loss of arterial elasticity and reduced arterial compliance and may subsequently lead to coronary artery disease.[29]
Sex
Men are at greater risk of heart disease than pre-menopausal women.[24][30] Once past menopause, it has been argued that a woman's risk is similar to a man's[30] although more recent data from the WHO and UN disputes this.[24] If a female has diabetes, she is more likely to develop heart disease than a male with diabetes.[31]
Coronary heart diseases are 2 to 5 times more common among middle-aged men than women.[28] In a study done by the World Health Organization, sex contributes to approximately 40% of the variation in sex ratios of coronary heart disease mortality.[32] Another study reports similar results finding that gender differences explains nearly half the risk associated with cardiovascular diseases[28] One of the proposed explanations for gender differences in cardiovascular diseases is hormonal difference.[28] Among women, estrogen is the predominant sex hormone. Estrogen may have protective effects on glucose metabolism and hemostatic system, and may have direct effect in improving endothelial cell function.[28] The production of estrogen decreases after menopause, and this may change the female lipid metabolism toward a more atherogenic form by decreasing the HDL cholesterol level while increasing LDL and total cholesterol levels.[28]
Among men and women, there are notable differences in body weight, height, body fat distribution, heart rate, stroke volume, and arterial compliance.[29] In the very elderly, age-related large artery pulsatility and stiffness is more pronounced among women than men.[29] This may be caused by the women's smaller body size and arterial dimensions which are independent of menopause.[29]
Tobacco
Cigarettes are the major form of smoked tobacco.[2] Risks to health from tobacco use result not only from direct consumption of tobacco, but also from exposure to second-hand smoke.[2] Approximately 10% of cardiovascular disease is attributed to smoking;[2] however, people who quit smoking by age 30 have almost as low a risk of death as never smokers.[33]
Physical inactivity
Insufficient physical activity (defined as less than 5 x 30 minutes of moderate activity per week, or less than 3 x 20 minutes of vigorous activity per week) is currently the fourth leading risk factor for mortality worldwide.[2] In 2008, 31.3% of adults aged 15 or older (28.2% men and 34.4% women) were insufficiently physically active.[2]
The risk of ischemic heart disease and diabetes mellitus is reduced by almost a third in adults who participate in 150 minutes of moderate physical activity each week (or equivalent).[34] In addition, physical activity assists weight loss and improves blood glucose control, blood pressure, lipid profile and insulin sensitivity. These effects may, at least in part, explain its cardiovascular benefits.[2]
Diet
High dietary intakes of saturated fat, trans-fats and salt, and low intake of fruits, vegetables and fish are linked to cardiovascular risk, although whether all these associations are a cause is disputed. The World Health Organization attributes approximately 1.7 million deaths worldwide to low fruit and vegetable consumption.[2] The amount of dietary salt consumed is also an important determinant of blood pressure levels and overall cardiovascular risk.[2] Frequent consumption of high-energy foods, such as processed foods that are high in fats and sugars, promotes obesity and may increase cardiovascular risk.[2] A Cochrane review found that replacing saturated fat with polyunsaturated fat (plant based oils) reduced cardiovascular disease risk. Cutting down on saturated fat reduced risk of cardiovascular disease by 17% including heart disease and stroke.[35]
High trans-fat intake has adverse effects on blood lipids and circulating inflammatory markers,[36] and elimination of trans-fat from diets has been widely advocated.[37][38] In 2018 the World Health Organization estimated that trans fats were the cause of more than half a million deaths per year.[38]
There is evidence that higher consumption of sugar is associated with higher blood pressure and unfavorable blood lipids,[39] and sugar intake also increases the risk of diabetes mellitus.[40] High consumption of processed meats is associated with an increased risk of cardiovascular disease, possibly in part due to increased dietary salt intake.[41]
The relationship between alcohol consumption and cardiovascular disease is complex, and may depend on the amount of alcohol consumed. There is a direct relationship between high levels of alcohol consumption and risk of cardiovascular disease.[2] Drinking at low levels without episodes of heavy drinking may be associated with a reduced risk of cardiovascular disease.[42]
Overall alcohol consumption at the population level is associated with multiple health risks that exceed any potential benefits.[2][43]
Sleep
Sleep disorders such as sleep disordered breathing and insomnia, as well as particularly short duration of sleep or particularly long duration of sleep, have been found to be associated with a higher cardiometabolic risk.[44]
Celiac disease
Untreated celiac disease can cause the development of many types of cardiovascular diseases, most of which improve or resolve with a gluten-free diet and intestinal healing. However, delays in recognition and diagnosis of celiac disease can cause irreversible heart damage.[17]
Socioeconomic disadvantage
Cardiovascular disease affects low- and middle-income countries even more than high-income countries.[45] There is relatively little information regarding social patterns of cardiovascular disease within low- and middle-income countries,[45] but within high-income countries low income and low educational status are consistently associated with greater risk of cardiovascular disease.[46] Policies that have resulted in increased socio-economic inequalities have been associated with greater subsequent socio-economic differences in cardiovascular disease[45] implying a cause and effect relationship. Psychosocial factors, environmental exposures, health behaviours, and health-care access and quality contribute to socio-economic differentials in cardiovascular disease.
[47] The Commission on Social Determinants of Health recommended that more equal distributions of power, wealth, education, housing, environmental factors, nutrition, and health care were needed to address inequalities in cardiovascular disease and non-communicable diseases.[48]
Air pollution
Particulate matter has been studied for its short- and long-term exposure effects on cardiovascular disease. Currently, PM2.5 is the major focus, in which gradients are used to determine CVD risk. For every 10 μg/m3 of PM2.5 long-term exposure, there was an estimated 8–18% CVD mortality risk.[49] Women had a higher relative risk (RR) (1.42) for PM2.5 induced coronary artery disease than men (0.90) did.[49] Overall, long-term PM exposure increased rate of atherosclerosis and inflammation. In regards to short-term exposure (2 hours), every 25 μg/m3 of PM2.5 resulted in a 48% increase of CVD mortality risk.[50] In addition, after only 5 days of exposure, a rise in systolic (2.8 mmHg) and diastolic (2.7 mmHg) blood pressure occurred for every 10.5 μg/m3 of PM2.5.[50] Other research has implicated PM2.5 in irregular heart rhythm, reduced heart rate variability (decreased vagal tone), and most notably heart failure.[50][51] PM2.5 is also linked to carotid artery thickening and increased risk of acute myocardial infarction.[50][51]
Cardiovascular risk assessment
Existing cardiovascular disease or a previous cardiovascular event, such as a heart attack or stroke, is the strongest predictor of a future cardiovascular event.[52] Age, sex, smoking, blood pressure, blood lipids and diabetes are important predictors of future cardiovascular disease in people who are not known to have cardiovascular disease.[53] These measures, and sometimes others, may be combined into composite risk scores to estimate an individual's future risk of cardiovascular disease.[52] Numerous risk scores exist although their respective merits are debated.[54] Other diagnostic tests and biomarkers remain under evaluation but currently these lack clear-cut evidence to support their routine use. They include family history, coronary artery calcification score, high sensitivity C-reactive protein (hs-CRP), ankle–brachial pressure index, lipoprotein subclasses and particle concentration, lipoprotein(a), apolipoproteins A-I and B, fibrinogen, white blood cell count, homocysteine, N-terminal pro B-type natriuretic peptide (NT-proBNP), and markers of kidney function.[55][56]High blood phosphorus is also linked to an increased risk.[57]
Occupational exposure
Little is known about the relationship between work and cardiovascular disease, but links have been established between certain toxins, extreme heat and cold, exposure to tobacco smoke, and mental health concerns such as stress and depression.[58]
Non-chemical risk factors
A 2015 SBU-report looking at non-chemical factors found an association for those:[59]
- with mentally stressful work with a lack of control over their working situation — with an effort-reward imbalance[59]
- who experience low social support at work; who experience injustice or experience insufficient opportunities for personal development; or those who experience job insecurity[59]
- those who work night schedules; or have long working weeks[59]
- those who are exposed to noise[59]
Specifically the risk of stroke was also increased by exposure to ionizing radiation.[59] Hypertension develops more often in those who experience job strain and who have shift-work.[59] Differences between women and men in risk are small, however men risk suffering and dying of heart attacks or stroke twice as often as women during working life.[59]
Chemical risk factors
A 2017 SBU report found evidence that workplace exposure to silica dust, engine exhaust or welding fumes is associated with heart disease.[60] Associations also exist for exposure to arsenic, benzopyrenes, lead, dynamite, carbon disulphide, carbon monoxide, metalworking fluids and occupational exposure to tobacco smoke.[60] Working with the electrolytic production of aluminium or the production of paper when the sulphate pulping process is used is associated with heart disease.[60] An association was also found between heart disease and exposure to compounds which are no longer permitted in certain work environments, such as phenoxy acids containing TCDD(dioxin) or asbestos.[60]
Workplace exposure to silica dust or asbestos is also associated with pulmonary heart disease.There is evidence that workplace exposure to lead, carbon disulphide, phenoxyacids containing TCDD, as well as working in an environment where aluminium is being electrolytically produced, is associated with stroke.[60]
Somatic mutations
As of 2017, evidence suggests that certain leukemia-associated mutations in blood cells may also lead to increased risk of cardiovascular disease. Several large-scale research projects looking at human genetic data have found a robust link between the presence of these mutations, a condition known as clonal hematopoiesis, and cardiovascular disease-related incidents and mortality.[61]
Pathophysiology

Density-Dependent Colour Scanning Electron Micrograph SEM (DDC-SEM) of cardiovascular calcification, showing in orange calcium phosphate spherical particles (denser material) and, in green, the extracellular matrix (less dense material)[62]
Population-based studies show that atherosclerosis, the major precursor of cardiovascular disease, begins in childhood. The Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study demonstrated that intimal lesions appear in all the aortas and more than half of the right coronary arteries of youths aged 7–9 years.[63]
This is extremely important considering that 1 in 3 people die from complications attributable to atherosclerosis. In order to stem the tide, education and awareness that cardiovascular disease poses the greatest threat, and measures to prevent or reverse this disease must be taken.
Obesity and diabetes mellitus are often linked to cardiovascular disease,[64] as are a history of chronic kidney disease and hypercholesterolaemia.[65] In fact, cardiovascular disease is the most life-threatening of the diabetic complications and diabetics are two- to four-fold more likely to die of cardiovascular-related causes than nondiabetics.[66][67][68]
Screening
Screening ECGs (either at rest or with exercise) are not recommended in those without symptoms who are at low risk.[69] This includes those who are young without risk factors.[70] In those at higher risk the evidence for screening with ECGs is inconclusive.[71] Additionally echocardiography, myocardial perfusion imaging, and cardiac stress testing is not recommended in those at low risk who do not have symptoms.[72] Some biomarkers may add to conventional cardiovascular risk factors in predicting the risk of future cardiovascular disease; however, the value of some biomarkers is questionable.[73][74]Ankle-brachial index (ABI), high-sensitivity C-reactive protein (hsCRP), and coronary artery calcium are also of unclear benefit in those without symptoms as of 2018.[75]
The NIH recommends lipid testing in children beginning at the age of 2 if there is a family history of heart disease or lipid problems.[76] It is hoped that early testing will improve lifestyle factors in those at risk such as diet and exercise.[77]
Screening and selection for primary prevention interventions has traditionally been done through absolute risk using a variety of scores (ex. Framingham or Reynolds risk scores).[78] This stratification has separated people who receive the lifestyle interventions (generally lower and intermediate risk) from the medication (higher risk). The number and variety of risk scores available for use has multiplied, but their efficacy according to a 2016 review was unclear due to lack of external validation or impact analysis.[79] Risk stratification models often lack sensitivity for population groups and do not account for the large number of negative events among the intermediate and low risk groups.[78] As a result, future preventative screening appears to shift toward applying prevention according to randomized trial results of each intervention rather than large-scale risk assessment.
Prevention
Up to 90% of cardiovascular disease may be preventable if established risk factors are avoided.[80][81] Currently practiced measures to prevent cardiovascular disease include:
Tobacco cessation and avoidance of second-hand smoke.[82] Smoking cessation reduces risk by about 35%.[83]- A low-fat, low-sugar, high-fiber diet including whole grains and fruit and vegetables.[82][84][85] Dietary interventions are effective in reducing cardiovascular risk factors over a year, but the longer term effects of such interventions and their impact on cardiovascular disease events is uncertain.[86]
- At least 150 minutes (2 hours and 30 minutes) of moderate exercise per week.[87][88] Exercise-based cardiac rehabilitation reduces risk of subsequent cardiovascular events by 26%,[89][needs update] but there have been few high quality studies of the benefits of exercise training in people with increased cardiovascular risk but no history of cardiovascular disease.[90]
- Limit alcohol consumption to the recommended daily limits;[82] People who moderately consume alcoholic drinks have a 25–30% lower risk of cardiovascular disease.[91][92] However, people who are genetically predisposed to consume less alcohol have lower rates of cardiovascular disease[93] suggesting that alcohol itself may not be protective. Excessive alcohol intake increases the risk of cardiovascular disease[94][92] and consumption of alcohol is associated with increased risk of a cardiovascular event in the day following consumption.[92]
- Lower blood pressure, if elevated. A 10 mmHg reduction in blood pressure reduces risk by about 20%.[95]
- Decrease non-HDL cholesterol.[96][97]Statin treament reduces cardiovascular mortality by about 31%.[98]
- Decrease body fat if overweight or obese.[99] The effect of weight loss is often difficult to distinguish from dietary change, and evidence on weight reducing diets is limited.[100] In observational studies of people with severe obesity, weight loss following bariatric surgery is associated with a 46% reduction in cardiovascular risk.[101]
- Decrease psychosocial stress.[102] This measure may be complicated by imprecise definitions of what constitute psychosocial interventions.[103] Mental stress–induced myocardial ischemia is associated with an increased risk of heart problems in those with previous heart disease.[104] Severe emotional and physical stress leads to a form of heart dysfunction known as Takotsubo syndrome in some people.[105] Stress, however, plays a relatively minor role in hypertension.[106] Specific relaxation therapies are of unclear benefit.[107][108]
Most guidelines recommend combining preventive strategies. A 2015 Cochrane Review found some evidence that interventions aiming to reduce more than one cardiovascular risk factor may have beneficial effects on blood pressure, body mass index and waist circumference; however, evidence was limited and the authors were unable to draw firm conclusions on the effects on cardiovascular events and mortality.[109] For adults without a known diagnosis of hypertension, diabetes, hyperlipidemia, or cardiovascular disease, routine counseling to advise them to improve their diet and increase their physical activity has not been found to significantly alter behavior, and thus is not recommended.[110] Another Cochrane review suggested that simply providing people with a cardiovascular disease risk score may reduce cardiovascular disease risk factors by a small amount compared to usual care.[111] However, there was some uncertainty as to whether providing these scores had any effect on cardiovascular disease events. It is unclear whether or not dental care in those with periodontitis affects their risk of cardiovascular disease.[112][needs update]
Diet
A diet high in fruits and vegetables decreases the risk of cardiovascular disease and death.[113] Evidence suggests that the Mediterranean diet may improve cardiovascular outcomes.[114] There is also evidence that a Mediterranean diet may be more effective than a low-fat diet in bringing about long-term changes to cardiovascular risk factors (e.g., lower cholesterol level and blood pressure).[115] The DASH diet (high in nuts, fish, fruits and vegetables, and low in sweets, red meat and fat) has been shown to reduce blood pressure,[116] lower total and low density lipoprotein cholesterol[117] and improve metabolic syndrome;[118] but the long-term benefits outside the context of a clinical trial have been questioned.[119] A high fiber diet appears to lower the risk.[120]
Total fat intake does not appear to be an important risk factor.[121][122] A diet high in trans fatty acids, however, does increase rates of cardiovascular disease.[122][123] Worldwide, dietary guidelines recommend a reduction in saturated fat.[124] However, there are some questions around the effect of saturated fat on cardiovascular disease in the medical literature.[123][125] Reviews from 2014 and 2015 did not find evidence of harm from saturated fats.[123][125] A 2012 Cochrane review found suggestive evidence of a small benefit from replacing dietary saturated fat by unsaturated fat.[126] A 2013 meta analysis concludes that substitution with omega 6 linoleic acid (a type of unsaturated fat) may increase cardiovascular risk.[124] Replacement of saturated fats with carbohydrates does not change or may increase risk.[127][128] Benefits from replacement with polyunsaturated fat appears greatest;[122][129] however, supplementation with omega-3 fatty acids (a type of polysaturated fat) does not appear to have an effect.[130][131]
A 2014 Cochrane review found unclear benefit of recommending a low-salt diet in people with high or normal blood pressure.[132] In those with heart failure, after one study was left out, the rest of the trials show a trend to benefit.[133][134] Another review of dietary salt concluded that there is strong evidence that high dietary salt intake increases blood pressure and worsens hypertension, and that it increases the number of cardiovascular disease events; both as a result of the increased blood pressure and, quite likely, through other mechanisms.[135][136] Moderate evidence was found that high salt intake increases cardiovascular mortality; and some evidence was found for an increase in overall mortality, strokes, and left ventricular hypertrophy.[135]
Medication
Blood pressure medication reduces cardiovascular disease in people at risk,[95] irrespective of age,[137] the baseline level of cardiovascular risk,[138] or baseline blood pressure.[139] The commonly-used drug regimens have similar efficacy in reducing the risk of all major cardiovascular events, although there may be differences between drugs in their ability to prevent specific outcomes.[140] Larger reductions in blood pressure produce larger reductions in risk,[140] and most people with high blood pressure require more than one drug to achieve adequate reduction in blood pressure.[141]
Statins are effective in preventing further cardiovascular disease in people with a history of cardiovascular disease.[142] As the event rate is higher in men than in women, the decrease in events is more easily seen in men than women.[142] In those at risk, but without a history of cardiovascular disease (primary prevention), statins decrease the risk of death and combined fatal and non-fatal cardiovascular disease.[143] The benefit, however, is small.[144] A United States guideline recommends statins in those who have a 12% or greater risk of cardiovascular disease over the next ten years.[145]Niacin, fibrates and CETP Inhibitors, while they may increase HDL cholesterol do not affect the risk of cardiovascular disease in those who are already on statins.[146]
Anti-diabetic medication may reduce cardiovascular risk in people with Type 2 Diabetes, although evidence is not conclusive.[147] A meta-analysis in 2009 including 27,049 participants and 2,370 major vascular events showed a 15% relative risk reduction in cardiovascular disease with more-intensive glucose lowering over an average follow-up period of 4.4 years, but an increased risk of major hypoglycemia.[148]
Aspirin has been found to be of only modest benefit in those at low risk of heart disease as the risk of serious bleeding is almost equal to the benefit with respect to cardiovascular problems.[149] In those at very low risk it is not recommended.[150] The United States Preventive Services Task Force recommends against use of aspirin for prevention in women less than 55 and men less than 45 years old; however, in those who are older it is recommends in some individuals.[151]
The use of vasoactive agents for people with pulmonary hypertension with left heart disease or hypoxemic lung diseases may cause harm and unnecessary expense.[152]
Physical activity
A systematic review estimated that inactivity is responsible for 6% of the burden of disease from coronary heart disease worldwide.[153] The authors estimated that 121,000 deaths from coronary heart disease could have been averted in Europe in 2008, if physical inactivity had been removed. A Cochrane review found some evidence that yoga has beneficial effects on blood pressure and cholesterol, but studies included in this review were of low quality.[154]
Dietary supplements
While a healthy diet is beneficial, the effect of antioxidant supplementation (vitamin E, vitamin C, etc.) or vitamins has not been shown to protect against cardiovascular disease and in some cases may possibly result in harm.[155][156][157] Mineral supplements have also not been found to be useful.[158]Niacin, a type of vitamin B3, may be an exception with a modest decrease in the risk of cardiovascular events in those at high risk.[159][160]Magnesium supplementation lowers high blood pressure in a dose dependent manner.[161] Magnesium therapy is recommended for people with ventricular arrhythmia associated with torsades de pointes who present with long QT syndrome as well as for the treatment of people with digoxin intoxication-induced arrhythmias.[162] There is no evidence to support omega-3 fatty acid supplementation.[163]
Management
Cardiovascular disease is treatable with initial treatment primarily focused on diet and lifestyle interventions.[2]Influenza may make heart attacks and strokes more likely and therefore influenza vaccination may decrease the chance of cardiovascular events and death in people with heart disease.[164]
Proper CVD management necessitates a focus on MI and stroke cases due to their combined high mortality rate, keeping in mind the cost-effectiveness of any intervention, especially in developing countries with low or middle income levels.[78] Regarding MI, strategies using aspirin, atenolol, streptokinase or tissue plasminogen activator have been compared for quality-adjusted life-year (QALY) in regions of low and middle income. The costs for a single QALY for aspirin, atenolol, streptokinase, and t-PA were $25, $630–$730, and $16,000, respectively. Aspirin, ACE inhibitors, beta blockers, and statins used together for secondary CVD prevention in the same regions showed single QALY costs of $300–400.
Epidemiology
Cardiovascular diseases deaths per million persons in 2012
318–925
926–1,148
1,149–1,294
1,295–1,449
1,450–1,802
1,803–2,098
2,099–2,624
2,625–3,203
3,204–5,271
5,272–10233
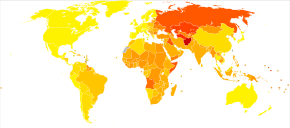
Disability-adjusted life year for cardiovascular diseases per 100,000 inhabitants in 2004[12]
no data
<900
900–1650
1650–2300
2300–3000
3000–3700
3700–4400
4400–5100
5100–5800
5800–6500
6500–7200
7200–7900
>7900
Cardiovascular diseases are the leading cause of death worldwide and in all regions except Africa.[165] In 2008, 30% of all global death was attributed to cardiovascular diseases. Death caused by cardiovascular diseases are also higher in low- and middle-income countries as over 80% of all global deaths caused by cardiovascular diseases occurred in those countries. It is also estimated that by 2030, over 23 million people will die from cardiovascular diseases each year.
It is estimated that 60% of the world's cardiovascular disease burden will occur in the South Asian subcontinent despite only accounting for 20% of the world's population. This may be secondary to a combination of genetic predisposition and environmental factors. Organizations such as the Indian Heart Association are working with the World Heart Federation to raise awareness about this issue.[166]
Research
There is evidence that cardiovascular disease existed in pre-history,[167] and research into cardiovascular disease dates from at least the 18th century.[168] The causes, prevention, and/or treatment of all forms of cardiovascular disease remain active fields of biomedical research, with hundreds of scientific studies being published on a weekly basis.
Recent areas of research include the link between inflammation and atherosclerosis[169] the potential for novel therapeutic interventions,[170] and the genetics of coronary heart disease.[171]
References
^ ab Go, AS; Mozaffarian, D; Roger, VL; Benjamin, EJ; Berry, JD; Borden, WB; Bravata, DM; Dai, S; Ford, ES; Fox, CS; Franco, S; Fullerton, HJ; Gillespie, C; Hailpern, SM; Heit, JA; Howard, VJ; Huffman, MD; Kissela, BM; Kittner, SJ; Lackland, DT; Lichtman, JH; Lisabeth, LD; Magid, D; Marcus, GM; Marelli, A; Matchar, DB; McGuire, DK; Mohler, ER; Moy, CS; Mussolino, ME; Nichol, G; Paynter, NP; Schreiner, PJ; Sorlie, PD; Stein, J; Turan, TN; Virani, SS; Wong, ND; Woo, D; Turner, MB; American Heart Association Statistics Committee and Stroke Statistics, Subcommittee (1 January 2013). "Heart disease and stroke statistics--2013 update: a report from the American Heart Association". Circulation. 127 (1): e6–e245. doi:10.1161/cir.0b013e31828124ad. PMC 5408511. PMID 23239837..mw-parser-output cite.citationfont-style:inherit.mw-parser-output qquotes:"""""""'""'".mw-parser-output code.cs1-codecolor:inherit;background:inherit;border:inherit;padding:inherit.mw-parser-output .cs1-lock-free abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-lock-limited a,.mw-parser-output .cs1-lock-registration abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-lock-subscription abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registrationcolor:#555.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration spanborder-bottom:1px dotted;cursor:help.mw-parser-output .cs1-hidden-errordisplay:none;font-size:100%.mw-parser-output .cs1-visible-errorfont-size:100%.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-formatfont-size:95%.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-leftpadding-left:0.2em.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-rightpadding-right:0.2em
^ abcdefghijklmnopqrstuvwxyzaaab Shanthi Mendis; Pekka Puska; Bo Norrving; World Health Organization (2011). Global Atlas on Cardiovascular Disease Prevention and Control (PDF). World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. pp. 3–18. ISBN 978-92-4-156437-3. Archived (PDF) from the original on 2014-08-17.
^ abc GBD 2013 Mortality and Causes of Death Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
^ ab GBD 2015 Mortality and Causes of Death Collaborators (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
^ McGill HC, McMahan CA, Gidding SS (March 2008). "Preventing heart disease in the 21st century: implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study". Circulation. 117 (9): 1216–27. doi:10.1161/CIRCULATIONAHA.107.717033. PMID 18316498.
^ Spinks, A; Glasziou, PP; Del Mar, CB (5 November 2013). "Antibiotics for sore throat". The Cochrane Database of Systematic Reviews. 11 (11): CD000023. doi:10.1002/14651858.CD000023.pub4. PMID 24190439.
^ Sutcliffe, P; Connock, M; Gurung, T; Freeman, K; Johnson, S; Ngianga-Bakwin, K; Grove, A; Gurung, B; Morrow, S; Stranges, S; Clarke, A (2013). "Aspirin in primary prevention of cardiovascular disease and cancer: a systematic review of the balance of evidence from reviews of randomized trials". PLOS ONE. 8 (12): e81970. doi:10.1371/journal.pone.0081970. PMC 3855368. PMID 24339983.
^ Sutcliffe, P; Connock, M; Gurung, T; Freeman, K; Johnson, S; Kandala, NB; Grove, A; Gurung, B; Morrow, S; Clarke, A (September 2013). "Aspirin for prophylactic use in the primary prevention of cardiovascular disease and cancer: a systematic review and overview of reviews". Health Technology Assessment. 17 (43): 1–253. doi:10.3310/hta17430. PMC 4781046. PMID 24074752.
^ ab Institute of Medicine of the National Academies (2010). "Epidemiology of Cardiovascular Disease". In Fuster, Valentin; Kelly, Bridget B. Promoting cardiovascular health in the developing world : a critical challenge to achieve global health. Washington, D.C.: National Academies Press. ISBN 978-0-309-14774-3. Archived from the original on 2017-09-08.
^ Moran, AE; Forouzanfar, MH; Roth, GA; Mensah, GA; Ezzati, M; Murray, CJ; Naghavi, M (8 April 2014). "Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the Global Burden of Disease 2010 study". Circulation. 129 (14): 1483–92. doi:10.1161/circulationaha.113.004042. PMC 4181359. PMID 24573352.
^ Mendis, Shanthi; Puska, Pekka; Norrving, Bo (2011). Global atlas on cardiovascular disease prevention and control (1 ed.). Geneva: World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. p. 48. ISBN 9789241564373.
^ ab "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 2009-11-11. Retrieved Nov 11, 2009.
^ Bridget B. Kelly; Institute of Medicine; Fuster, Valentin (2010). Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Washington, D.C: National Academies Press. ISBN 978-0-309-14774-3.
^ Finks, SW; Airee, A; Chow, SL; Macaulay, TE; Moranville, MP; Rogers, KC; Trujillo, TC (April 2012). "Key articles of dietary interventions that influence cardiovascular mortality". Pharmacotherapy. 32 (4): e54–87. doi:10.1002/j.1875-9114.2011.01087.x. PMID 22392596.
^ Micha, R; Michas, G; Mozaffarian, D (Dec 2012). "Unprocessed red and processed meats and risk of coronary artery disease and type 2 diabetes—an updated review of the evidence". Current Atherosclerosis Reports. 14 (6): 515–24. doi:10.1007/s11883-012-0282-8. PMC 3483430. PMID 23001745.
^ Shanthi Mendis; Pekka Puska; Bo Norrving (2011). Global Atlas on Cardiovascular Disease Prevention and Control. World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. ISBN 978-92-4-156437-3. Archived from the original on 2016-05-06.
^ ab Ciaccio EJ, Lewis SK, Biviano AB, Iyer V, Garan H, Green PH (2017). "Cardiovascular involvement in celiac disease". World J Cardiol (Review). 9 (8): 652–666. doi:10.4330/wjc.v9.i8.652. PMC 5583538. PMID 28932354.
^ Yusuf S, Hawken S, Ounpuu S, et al. (2004). "Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study". Lancet. 364 (9438): 937–52. doi:10.1016/S0140-6736(04)17018-9. PMID 15364185.
^ ab McPhee, Stephen (2012). Current medical diagnosis & treatment 2012. New York: McGraw-Hill Medical. p. 430. ISBN 9780071763721.
^ Eckel, Robert H. (November 4, 1997). "Obesity and Heart Disease: A Statement for Healthcare Professionals From the Nutrition Committee, American Heart Association". Circulation. 96 (9): 3248–3250. doi:10.1161/01.CIR.96.9.3248. Archived from the original on 2017-07-01.
^ Kathiresan, S; Srivastava, D (16 March 2012). "Genetics of human cardiovascular disease". Cell. 148 (6): 1242–57. doi:10.1016/j.cell.2012.03.001. PMC 3319439. PMID 22424232.
^ Nikpay, Majid; Goel, Anuj; Won, Hong-Hee; Hall, Leanne M; Willenborg, Christina; Kanoni, Stavroula; Saleheen, Danish; Kyriakou, Theodosios; Nelson, Christopher P (2015). "A comprehensive 1000 Genomes–based genome-wide association meta-analysis of coronary artery disease". Nature Genetics. 47 (10): 1121–1130. doi:10.1038/ng.3396. PMC 4589895. PMID 26343387.
^ ab MacRae, Calum A.; Vasan, Ramachandran S. (2016-06-21). "The Future of Genetics and Genomics: Closing the Phenotype Gap in Precision Medicine". Circulation. 133 (25): 2634–2639. doi:10.1161/CIRCULATIONAHA.116.022547. ISSN 1524-4539. PMC 6188655. PMID 27324359.
^ abc Finegold, JA; Asaria, P; Francis, DP (Dec 4, 2012). "Mortality from ischaemic heart disease by country, region, and age: Statistics from World Health Organisation and United Nations". International Journal of Cardiology. 168 (2): 934–945. doi:10.1016/j.ijcard.2012.10.046. PMC 3819990. PMID 23218570.
^ D'Adamo, E; Guardamagna, O; Chiarelli, F; Bartuli, A; Liccardo, D; Ferrari, F; Nobili, V (2015). "Atherogenic dyslipidemia and cardiovascular risk factors in obese children". International Journal of Endocrinology. 2015: 1–9. doi:10.1155/2015/912047. PMC 4309297. PMID 25663838.
^ "Understand Your Risk of Heart Attack". American Heart Association.http://www.heart.org/HEARTORG/Conditions/HeartAttack/UnderstandYourRiskofHeartAttack/Understand-Your-Risk-of-Heart-Attack_UCM_002040_Article.jsp#
^ Mackay, Mensah, Mendis, et al. The Atlas of Heart Disease and Stroke. World Health Organization. January 2004.
^ abcdefg Jousilahti Vartiainen; Tuomilehto Puska (1999). "Sex, Age, Cardiovascular Risk Factors, and coronary heart disease". Circulation. 99 (9): 1165–1172. doi:10.1161/01.cir.99.9.1165.
^ abcd Jani B, Rajkumar C (2006). "Ageing and vascular ageing". Postgrad Med J. 82 (968): 357–362. doi:10.1136/pgmj.2005.036053. PMC 2563742. PMID 16754702.
^ ab "Risk factors". Archived from the original on 2012-05-10. Retrieved 2012-05-03.
^ "Diabetes raises women's risk of heart disease more than for men". NPR.org. May 22, 2014. Archived from the original on May 23, 2014. Retrieved May 23, 2014.
^ Jackson R, Chambles L, Higgins M, Kuulasmaa K, Wijnberg L, Williams D (WHO MONICA Project, and ARIC Study.) Sex difference in ischaemic heart disease mortality and risk factors in 46 communities: an ecologic analysis. Cardiovasc Risk Factors. 1999; 7:43–54.
^ Richard Doll; Richard Peto; Jillian Boreham & Isabelle Sutherland (June 2004). "Mortality in relation to smoking: 50 years' observations on male British doctors". BMJ. 328 (7455): 1519. doi:10.1136/bmj.38142.554479.AE. PMC 437139. PMID 15213107.
^ World Health Organization; UNAIDS (1 January 2007). Prevention of Cardiovascular Disease. World Health Organization. pp. 3–. ISBN 978-92-4-154726-0. Archived from the original on 27 April 2016.
^ Hooper, Lee; Martin, Nicole; Abdelhamid, Asmaa; Davey Smith, George (2015-06-10). "Reduction in saturated fat intake for cardiovascular disease". The Cochrane Database of Systematic Reviews. 6 (6): CD011737. doi:10.1002/14651858.CD011737. ISSN 1469-493X. PMID 26068959.
^ Booker, C.S.; Mann, J.I. (2008). "Trans fatty acids and cardiovascular health: Translation of the evidence base". Nutrition, Metabolism and Cardiovascular Diseases. 18 (6): 448–456. doi:10.1016/j.numecd.2008.02.005. ISSN 0939-4753. PMID 18468872.
^ Remig, Valentina; Franklin, Barry; Margolis, Simeon; Kostas, Georgia; Nece, Theresa; Street, James C. (2010). "Trans Fats in America: A Review of Their Use, Consumption, Health Implications, and Regulation". Journal of the American Dietetic Association. 110 (4): 585–592. doi:10.1016/j.jada.2009.12.024. hdl:2097/6377. ISSN 0002-8223. PMID 20338284.
^ ab "WHO plan to eliminate industrially-produced trans-fatty acids from global food supply". World Health Organization. Retrieved 15 May 2018.
^ Te Morenga, L. A.; Howatson, A. J.; Jones, R. M.; Mann, J. (2014). "Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids". American Journal of Clinical Nutrition. 100 (1): 65–79. doi:10.3945/ajcn.113.081521. ISSN 0002-9165. PMID 24808490.
^ "Wylie-Rosett2002"
^ Micha, Renata; Michas, Georgios; Mozaffarian, Dariush (2012). "Unprocessed Red and Processed Meats and Risk of Coronary Artery Disease and Type 2 Diabetes – An Updated Review of the Evidence". Current Atherosclerosis Reports. 14 (6): 515–524. doi:10.1007/s11883-012-0282-8. ISSN 1523-3804. PMC 3483430. PMID 23001745.
^ Mukamal, Kenneth J.; Chen, Chiung M.; Rao, Sowmya R.; Breslow, Rosalind A. (2010). "Alcohol Consumption and Cardiovascular Mortality Among U.S. Adults, 1987 to 2002". Journal of the American College of Cardiology. 55 (13): 1328–1335. doi:10.1016/j.jacc.2009.10.056. ISSN 0735-1097. PMC 3865979. PMID 20338493.
^ World Health Organization (2011). Global Status Report on Alcohol and Health. World Health Organization. ISBN 978-92-4-156415-1. Archived from the original on 2016-05-07.
^ St-Onge MP, Grandner MA, Brown D, Conroy MB, Jean-Louis G, Coons M, Bhatt DL (November 2016). "Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement From the American Heart Association". Circulation (Review). 134 (18): e367–e386. doi:10.1161/CIR.0000000000000444. PMC 5567876. PMID 27647451.
^ abc Mariachiara Di Cesare; Young-Ho Khang; Perviz Asaria; Tony Blakely; Melanie J. Cowan; Farshad Farzadfar; Ramiro Guerrero; Nayu Ikeda; Catherine Kyobutungi; Kelias P. Msyamboza; Sophal Oum; John W. Lynch; Michael G. Marmot; Majid Ezzati (February 2013). "Inequalities in non-communicable diseases and effective responses". Lancet. 381 (9866): 585–597. doi:10.1016/S0140-6736(12)61851-0. PMID 23410608.
^ J. P. Mackenbach; A. E. Cavelaars; A. E. Kunst; F. Groenhof (July 2000). "Socioeconomic inequalities in cardiovascular disease mortality; an international study". European Heart Journal. 21 (14): 1141–1151. doi:10.1053/euhj.1999.1990. PMID 10924297.
^ Alexander M. Clark; Marie DesMeules; Wei Luo; Amanda S. Duncan; Andy Wielgosz (November 2009). "Socioeconomic status and cardiovascular disease: risks and implications for care". Nature Reviews Cardiology. 6 (11): 712–722. doi:10.1038/nrcardio.2009.163. PMID 19770848.
^ World Health Organization (2008). Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health : Commission on Social Determinants of Health Final Report. World Health Organization. pp. 26–. ISBN 978-92-4-156370-3. Archived from the original on 2016-05-01.
^ ab Khallaf, Mohamed (2011). The Impact of Air Pollution on Health, Economy, Environment and Agricultural Sources. InTech. pp. 69–92. ISBN 978-953-307-528-0.
^ abcd Franchini M, Mannucci PM (2012). "Air pollution and cardiovascular disease". Thrombosis Research. 129 (3): 230–4. doi:10.1016/j.thromres.2011.10.030. PMID 22113148.
^ ab Sun Q, Hong X, Wold LE (2010). "Cardiovascular Effects of Ambient Particulate Air Pollution Exposure". Circulation. 121 (25): 2755–65. doi:10.1161/CIRCULATIONAHA.109.893461. PMC 2924678. PMID 20585020.
^ ab Tunstall-Pedoe, H. (2011). "Cardiovascular Risk and Risk Scores: ASSIGN, Framingham, QRISK and others: how to choose". Heart. 97 (6): 442–444. doi:10.1136/hrt.2010.214858. ISSN 1355-6037. PMID 21339319.
^ World Health Organization (2007). Prevention of Cardiovascular Disease: Guidelines for Assessment and Management of Cardiovascular Risk. World Health Organization. ISBN 978-92-4-154717-8. Archived from the original on 2016-05-06.
^ Hernandez, Adrian V.; van Staa, Tjeerd-Pieter; Gulliford, Martin; Ng, Edmond S.-W.; Goldacre, Ben; Smeeth, Liam (2014). "Prediction of Cardiovascular Risk Using Framingham, ASSIGN and QRISK2: How Well Do They Predict Individual Rather than Population Risk?". PLoS ONE. 9 (10): e106455. doi:10.1371/journal.pone.0106455. ISSN 1932-6203. PMC 4182667. PMID 25271417.
^ Hlatky, M. A.; Greenland, P.; Arnett, D. K.; Ballantyne, C. M.; Criqui, M. H.; Elkind, M. S.V.; Go, A. S.; Harrell, F. E.; Hong, Y.; Howard, B. V.; Howard, V. J.; Hsue, P. Y.; Kramer, C. M.; McConnell, J. P.; Normand, S.-L. T.; O'Donnell, C. J.; Smith, S. C.; Wilson, P. W.F. (2009). "Criteria for Evaluation of Novel Markers of Cardiovascular Risk: A Scientific Statement From the American Heart Association". Circulation. 119 (17): 2408–2416. doi:10.1161/CIRCULATIONAHA.109.192278. ISSN 0009-7322. PMC 2956982. PMID 19364974.
^ Eckel, Robert H; Cornier, Marc-Andre (2014). "Update on the NCEP ATP-III emerging cardiometabolic risk factors". BMC Medicine. 12 (1): 115. doi:10.1186/1741-7015-12-115. ISSN 1741-7015. PMC 4283079. PMID 25154373.
^ Bai, W; Li, J; Liu, J (1 October 2016). "Serum phosphorus, cardiovascular and all-cause mortality in the general population: A meta-analysis". Clinica Chimica Acta. 461: 76–82. doi:10.1016/j.cca.2016.07.020. PMID 27475981.
^ "CDC - NIOSH Program Portfolio : Cancer, Reproductive, and Cardiovascular Diseases : Program Description". www.cdc.gov. Archived from the original on 2016-05-15. Retrieved 2016-06-07.
^ abcdefgh Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU) (2015-08-26). "Occupational Exposures and Cardiovascular Disease". www.sbu.se. Archived from the original on 2017-06-14. Retrieved 2017-06-01.
^ abcde Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU). "Occupational health and safety – chemical exposure". www.sbu.se. Archived from the original on 2017-06-06. Retrieved 2017-06-01.
^ Jan, M; Ebert, BL; Jaiswal, S (January 2017). "Clonal hematopoiesis". Seminars in Hematology. 54 (1): 43–50. doi:10.1053/j.seminhematol.2016.10.002. PMID 28088988.
^ Bertazzo S.; et al. (2013). "Nano-analytical electron microscopy reveals fundamental insights into human cardiovascular tissue calcification". Nature Materials. 12 (6): 576–583. doi:10.1038/nmat3627. PMC 5833942. PMID 23603848.CS1 maint: Explicit use of et al. (link)
^ Vanhecke TE, Miller WM, Franklin BA, Weber JE, McCullough PA (Oct 2006). "Awareness, knowledge, and perception of heart disease among adolescents". Eur J Cardiovasc Prev Rehabil. 13 (5): 718–23. doi:10.1097/01.hjr.0000214611.91490.5e. PMID 17001210.
^ Highlander P, Shaw GP (2010). "Current pharmacotherapeutic concepts for the treatment of cardiovascular disease in diabetics". Ther Adv Cardiovasc Dis. 4 (1): 43–54. doi:10.1177/1753944709354305. PMID 19965897.
^ NPS Medicinewise (1 March 2011). "NPS Prescribing Practice Review 53: Managing lipids". Archived from the original on 19 March 2011. Retrieved 1 August 2011.
^ Kvan E.; Pettersen K.I.; Sandvik L.; Reikvam A. (2007). "High mortality in diabetic patient with acute myocardial infarction: cardiovascular co-morbidities contribute most to the high risk". Int J Cardiol. 121 (2): 184–188. doi:10.1016/j.ijcard.2006.11.003. PMID 17184858.
^ Norhammar A.; Malmberg K.; Diderhol E.; Lagerqvist B.; Lindahl B., Ryde; et al. (2004). "Diabetes mellitus: the major risk factor in unstable coronary artery disease even after consideration of the extent of coronary artery disease and benefits of revascularization. J". Am Coll Cardiol. 43 (4): 585–591. doi:10.1016/j.jacc.2003.08.050. PMID 14975468.
^ DECODE, European Diabetes Epidemiology Group (1999). "Glucose tolerance and mortality: comparison of WHO and American Diabetes Association diagnostic criteria". Lancet. 354 (9179): 617–621. doi:10.1016/S0140-6736(98)12131-1. PMID 10466661.
^ US Preventive Services Task, Force.; Curry, SJ; Krist, AH; Owens, DK; Barry, MJ; Caughey, AB; Davidson, KW; Doubeni, CA; Epling JW, Jr; Kemper, AR; Kubik, M; Landefeld, CS; Mangione, CM; Silverstein, M; Simon, MA; Tseng, CW; Wong, JB (12 June 2018). "Screening for Cardiovascular Disease Risk With Electrocardiography: US Preventive Services Task Force Recommendation Statement". JAMA. 319 (22): 2308–2314. doi:10.1001/jama.2018.6848. PMID 29896632.
^ Maron, B. J.; Friedman, R. A.; Kligfield, P.; Levine, B. D.; Viskin, S.; Chaitman, B. R.; Okin, P. M.; Saul, J. P.; Salberg, L.; Van Hare, G. F.; Soliman, E. Z.; Chen, J.; Matherne, G. P.; Bolling, S. F.; Mitten, M. J.; Caplan, A.; Balady, G. J.; Thompson, P. D. (15 September 2014). "Assessment of the 12-Lead ECG as a Screening Test for Detection of Cardiovascular Disease in Healthy General Populations of Young People (12–25 Years of Age): A Scientific Statement From the American Heart Association and the American College of Cardiology". Circulation. 130 (15): 1303–1334. doi:10.1161/CIR.0000000000000025. PMID 25223981.
^ Moyer, VA; U.S. Preventive Services Task Force (Oct 2, 2012). "Screening for coronary heart disease with electrocardiography: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 157 (7): 512–8. doi:10.7326/0003-4819-157-7-201210020-00514. PMID 22847227.
^ Chou, Roger (17 March 2015). "Cardiac Screening With Electrocardiography, Stress Echocardiography, or Myocardial Perfusion Imaging: Advice for High-Value Care From the American College of Physicians". Annals of Internal Medicine. 162 (6): 438–47. doi:10.7326/M14-1225. PMID 25775317.
^ Wang TJ, Gona P, Larson MG, Tofler GH, Levy D, Newton-Cheh C, Jacques PF, Rifai N, Selhub J, Robins SJ, Benjamin EJ, D'Agostino RB, Vasan RS (2006). "Multiple biomarkers for the prediction of first major cardiovascular events and death". N. Engl. J. Med. 355 (25): 2631–billy bob joe9. doi:10.1056/NEJMoa055373. PMID 17182988.
^ Spence JD (2006). "Technology Insight: ultrasound measurement of carotid plaque—patient management, genetic research, and therapy evaluation". Nat Clin Pract Neurol. 2 (11): 611–9. doi:10.1038/ncpneuro0324. PMID 17057748.
^ US Preventive Services Task, Force.; Curry, SJ; Krist, AH; Owens, DK; Barry, MJ; Caughey, AB; Davidson, KW; Doubeni, CA; Epling JW, Jr; Kemper, AR; Kubik, M; Landefeld, CS; Mangione, CM; Silverstein, M; Simon, MA; Tseng, CW; Wong, JB (17 July 2018). "Risk Assessment for Cardiovascular Disease With Nontraditional Risk Factors: US Preventive Services Task Force Recommendation Statement". JAMA. 320 (3): 272–280. doi:10.1001/jama.2018.8359. PMID 29998297.
^ Adolescents, Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children And (2011-12-01). "Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: Summary Report". Pediatrics. 128 (Supplement 5): S213–S256. doi:10.1542/peds.2009-2107C. ISSN 0031-4005. PMC 4536582. PMID 22084329. Archived from the original on 2016-07-16.
^ Saenger, Amy K. (2012-08-01). "Universal Lipid Screening in Children and Adolescents: A Baby Step toward Primordial Prevention?". Clinical Chemistry. 58 (8): 1179–1181. doi:10.1373/clinchem.2012.182287. ISSN 0009-9147. PMID 22510399.
^ abc Mann, Douglas L. (2014). Braunwald's heart disease : a textbook of cardiovascular medicine. Mann, Douglas L.,, Zipes, Douglas P.,, Libby, Peter,, Bonow, Robert O.,, Braunwald, Eugene, 1929- (Tenth ed.). Philadelphia, PA. ISBN 9781455751334. OCLC 890409638.
^ Damen, Johanna A. A. G.; Hooft, Lotty; Schuit, Ewoud; Debray, Thomas P. A.; Collins, Gary S.; Tzoulaki, Ioanna; Lassale, Camille M.; Siontis, George C. M.; Chiocchia, Virginia (2016-05-16). "Prediction models for cardiovascular disease risk in the general population: systematic review". BMJ. 353: i2416. doi:10.1136/bmj.i2416. ISSN 1756-1833. PMC 4868251. PMID 27184143. Archived from the original on 2017-08-29.
^ McGill, Henry C.; McMahan, C. Alex; Gidding, Samuel S. (2008-03-04). "Preventing Heart Disease in the 21st Century". Circulation. 117 (9): 1216–1227. doi:10.1161/CIRCULATIONAHA.107.717033. ISSN 0009-7322. PMID 18316498.
^ McNeal, Catherine J.; Dajani, Tala; Wilson, Don; Cassidy-Bushrow, Andrea E.; Dickerson, Justin B.; Ory, Marcia (2010-01-01). "Hypercholesterolemia in youth: opportunities and obstacles to prevent premature atherosclerotic cardiovascular disease". Current Atherosclerosis Reports. 12 (1): 20–28. doi:10.1007/s11883-009-0072-0. ISSN 1534-6242. PMID 20425267.
^ abc NHS Direct Archived 2011-09-06 at the Wayback Machine.
^ Critchley, J.; Capewell, S. (2004-01-01). "Smoking cessation for the secondary prevention of coronary heart disease". The Cochrane Database of Systematic Reviews (1): CD003041. doi:10.1002/14651858.CD003041.pub2. ISSN 1469-493X. PMID 14974003.
^ Ignarro, LJ; Balestrieri, ML; Napoli, C (Jan 15, 2007). "Nutrition, physical activity, and cardiovascular disease: an update". Cardiovascular Research. 73 (2): 326–40. doi:10.1016/j.cardiores.2006.06.030. PMID 16945357.
^ Levy, L; Tedstone, A (20 February 2017). "UK Dietary Policy for the Prevention of Cardiovascular Disease". Healthcare. 5 (1): 9. doi:10.3390/healthcare5010009. PMC 5371915. PMID 28230719. Archived from the original on 13 March 2017.
^ Rees, Karen; Dyakova, Mariana; Wilson, Nicola; Ward, Kirsten; Thorogood, Margaret; Brunner, Eric (2013-12-06). "Dietary advice for reducing cardiovascular risk" (PDF). The Cochrane Database of Systematic Reviews (12): CD002128. doi:10.1002/14651858.CD002128.pub5. ISSN 1469-493X. PMID 24318424.
^ "Chapter 4: Active Adults". health.gov. Archived from the original on 2017-03-13.
^ "Physical activity guidelines for adults". NHS Choices. 2018-04-26. Archived from the original on 2017-02-19.
^ Heran Balraj S (2011). "Exercise‐based cardiac rehabilitation for coronary heart disease" (PDF). Cochrane Database of Systematic Reviews (7): CD001800. doi:10.1002/14651858.cd001800.pub2. PMC 4229995. PMID 21735386.
^ Seron, Pamela; Lanas, Fernando; Pardo Hernandez, Hector; Bonfill Cosp, Xavier (2014-08-13). "Exercise for people with high cardiovascular risk". The Cochrane Database of Systematic Reviews (8): CD009387. doi:10.1002/14651858.CD009387.pub2. ISSN 1469-493X. PMID 25120097.
^ Ronksley, Paul E.; Brien, Susan E.; Turner, Barbara J.; Mukamal, Kenneth J.; Ghali, William A. (2011-02-22). "Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis". BMJ. 342: d671. doi:10.1136/bmj.d671. ISSN 1756-1833. PMC 3043109. PMID 21343207.
^ abc Mostofsky, Elizabeth; Chahal, Harpreet S.; Mukamal, Kenneth J.; Rimm, Eric B.; Mittleman, Murray A. (2016-03-08). "Alcohol and Immediate Risk of Cardiovascular Events: A Systematic Review and Dose-Response Meta-Analysis". Circulation. 133 (10): 979–987. doi:10.1161/CIRCULATIONAHA.115.019743. ISSN 1524-4539. PMC 4783255. PMID 26936862.
^ Holmes, Michael V.; Dale, Caroline E.; Zuccolo, Luisa; Silverwood, Richard J.; Guo, Yiran; Ye, Zheng; Prieto-Merino, David; Dehghan, Abbas; Trompet, Stella (2014-07-10). "Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data". BMJ. 349: g4164. doi:10.1136/bmj.g4164. ISSN 1756-1833. PMC 4091648. PMID 25011450.
^ Klatsky AL (May 2009). "Alcohol and cardiovascular diseases". Expert Rev Cardiovasc Ther. 7 (5): 499–506. doi:10.1586/erc.09.22. PMID 19419257.
^ ab Ettehad, Dena; Emdin, Connor A.; Kiran, Amit; Anderson, Simon G.; Callender, Thomas; Emberson, Jonathan; Chalmers, John; Rodgers, Anthony; Rahimi, Kazem (2016-03-05). "Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis". Lancet. 387 (10022): 957–967. doi:10.1016/S0140-6736(15)01225-8. ISSN 1474-547X. PMID 26724178.
^ McMahan, C. Alex; Gidding, Samuel S.; Malcom, Gray T.; Tracy, Richard E.; Strong, Jack P.; McGill, Henry C. (2006-10-01). "Pathobiological determinants of atherosclerosis in youth risk scores are associated with early and advanced atherosclerosis". Pediatrics. 118 (4): 1447–1455. doi:10.1542/peds.2006-0970. ISSN 1098-4275. PMID 17015535.
^ Raitakari, Olli T.; Rönnemaa, Tapani; Järvisalo, Mikko J.; Kaitosaari, Tuuli; Volanen, Iina; Kallio, Katariina; Lagström, Hanna; Jokinen, Eero; Niinikoski, Harri (2005-12-13). "Endothelial function in healthy 11-year-old children after dietary intervention with onset in infancy: the Special Turku Coronary Risk Factor Intervention Project for children (STRIP)". Circulation. 112 (24): 3786–3794. doi:10.1161/CIRCULATIONAHA.105.583195. ISSN 1524-4539. PMID 16330680.
^ Chou, Roger; Dana, Tracy; Blazina, Ian; Daeges, Monica; Jeanne, Thomas L. (2016-11-15). "Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force". JAMA. 316 (19): 2008–2024. doi:10.1001/jama.2015.15629. ISSN 1538-3598. PMID 27838722.
^ McTigue KM, Hess R, Ziouras J (September 2006). "Obesity in older adults: a systematic review of the evidence for diagnosis and treatment". Obesity. 14 (9): 1485–97. doi:10.1038/oby.2006.171. PMID 17030958.
^ Semlitsch, Thomas; Jeitler, Klaus; Berghold, Andrea; Horvath, Karl; Posch, Nicole; Poggenburg, Stephanie; Siebenhofer, Andrea (2016-03-02). "Long-term effects of weight-reducing diets in people with hypertension". The Cochrane Database of Systematic Reviews. 3: CD008274. doi:10.1002/14651858.CD008274.pub3. ISSN 1469-493X. PMID 26934541.
^ Kwok, Chun Shing; Pradhan, Ashish; Khan, Muhammad A.; Anderson, Simon G.; Keavney, Bernard D.; Myint, Phyo Kyaw; Mamas, Mamas A.; Loke, Yoon K. (2014-04-15). "Bariatric surgery and its impact on cardiovascular disease and mortality: a systematic review and meta-analysis". International Journal of Cardiology. 173 (1): 20–28. doi:10.1016/j.ijcard.2014.02.026. hdl:2164/3181. ISSN 1874-1754. PMID 24636546.
^ Linden W, Stossel C, Maurice J (April 1996). "Psychosocial interventions for patients with coronary artery disease: a meta-analysis". Arch. Intern. Med. 156 (7): 745–52. doi:10.1001/archinte.1996.00440070065008. PMID 8615707.
^ Thompson, D. R.; Ski, C. F. (2013). "Psychosocial interventions in cardiovascular disease - what are they?". European Journal of Preventive Cardiology. 20 (6): 916–917. doi:10.1177/2047487313494031. ISSN 2047-4873. PMID 24169589.
^ Wei, J; Rooks, C; Ramadan, R; Shah, AJ; Bremner, JD; Quyyumi, AA; Kutner, M; Vaccarino, V (15 July 2014). "Meta-analysis of mental stress-induced myocardial ischemia and subsequent cardiac events in patients with coronary artery disease". The American Journal of Cardiology. 114 (2): 187–92. doi:10.1016/j.amjcard.2014.04.022. PMC 4126399. PMID 24856319.
^ Pelliccia, F; Greco, C; Vitale, C; Rosano, G; Gaudio, C; Kaski, JC (August 2014). "Takotsubo syndrome (stress cardiomyopathy): an intriguing clinical condition in search of its identity". The American Journal of Medicine. 127 (8): 699–704. doi:10.1016/j.amjmed.2014.04.004. PMID 24754972.
^ Marshall, IJ; Wolfe, CD; McKevitt, C (Jul 9, 2012). "Lay perspectives on hypertension and drug adherence: systematic review of qualitative research". BMJ. 345: e3953. doi:10.1136/bmj.e3953. PMC 3392078. PMID 22777025.
^ Dickinson, HO; Mason, JM; Nicolson, DJ; Campbell, F; Beyer, FR; Cook, JV; Williams, B; Ford, GA (February 2006). "Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials". Journal of Hypertension. 24 (2): 215–33. doi:10.1097/01.hjh.0000199800.72563.26. PMID 16508562.
^ Abbott, RA; Whear, R; Rodgers, LR; Bethel, A; Thompson Coon, J; Kuyken, W; Stein, K; Dickens, C (May 2014). "Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials". Journal of Psychosomatic Research. 76 (5): 341–51. doi:10.1016/j.jpsychores.2014.02.012. PMID 24745774.
^ Uthman, Olalekan A.; Hartley, Louise; Rees, Karen; Taylor, Fiona; Ebrahim, Shah; Clarke, Aileen (2015-08-04). "Multiple risk factor interventions for primary prevention of cardiovascular disease in low- and middle-income countries". The Cochrane Database of Systematic Reviews (8): CD011163. doi:10.1002/14651858.CD011163.pub2. ISSN 1469-493X. PMID 26272648.
^ Moyer, VA; U.S. Preventive Services Task Force (September 4, 2012). "Behavioral counseling interventions to promote a healthful diet and physical activity for cardiovascular disease prevention in adults: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 157 (5): 367–71. doi:10.7326/0003-4819-157-5-201209040-00486. PMID 22733153.
^ Karmali, Kunal N.; Persell, Stephen D.; Perel, Pablo; Lloyd-Jones, Donald M.; Berendsen, Mark A.; Huffman, Mark D. (2017-03-14). "Risk scoring for the primary prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 3: CD006887. doi:10.1002/14651858.CD006887.pub4. ISSN 1469-493X. PMID 28290160.
^ Li, C; Lv, Z; Shi, Z; Zhu, Y; Wu, Y; Li, L; Iheozor-Ejiofor, Z (Aug 15, 2014). "Periodontal therapy for the management of cardiovascular disease in patients with chronic periodontitis". The Cochrane Database of Systematic Reviews. 8 (8): CD009197. doi:10.1002/14651858.CD009197.pub2. PMID 25123257.
^ Wang, X; Ouyang, Y; Liu, J; Zhu, M; Zhao, G; Bao, W; Hu, FB (Jul 29, 2014). "Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies". BMJ. 349: g4490. doi:10.1136/bmj.g4490. PMC 4115152. PMID 25073782.
^ Walker C, Reamy BV (April 2009). "Diets for cardiovascular disease prevention: what is the evidence?". Am Fam Physician. 79 (7): 571–8. PMID 19378874.
^ Nordmann, AJ; Suter-Zimmermann, K; Bucher, HC; Shai, I; Tuttle, KR; Estruch, R; Briel, M (September 2011). "Meta-analysis comparing Mediterranean to low-fat diets for modification of cardiovascular risk factors". The American Journal of Medicine. 124 (9): 841–51.e2. doi:10.1016/j.amjmed.2011.04.024. PMID 21854893. Archived from the original on 2013-12-20.
^ Sacks FM, Svetkey LP, Vollmer WM, et al. (January 2001). "Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group". N. Engl. J. Med. 344 (1): 3–10. doi:10.1056/NEJM200101043440101. PMID 11136953.
^ Obarzanek E, Sacks FM, Vollmer WM, et al. (July 2001). "Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) Trial". Am. J. Clin. Nutr. 74 (1): 80–9. doi:10.1093/ajcn/74.1.80. PMID 11451721.
^ Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi T, Azizi F (December 2005). "Beneficial effects of a Dietary Approaches to Stop Hypertension eating plan on features of the metabolic syndrome". Diabetes Care. 28 (12): 2823–31. doi:10.2337/diacare.28.12.2823. PMID 16306540.
^ Logan AG (March 2007). "DASH Diet: time for a critical appraisal?". Am. J. Hypertens. 20 (3): 223–4. doi:10.1016/j.amjhyper.2006.10.006. PMID 17324730.
^ Threapleton, D. E.; Greenwood, D. C.; Evans, C. E. L.; Cleghorn, C. L.; Nykjaer, C.; Woodhead, C.; Cade, J. E.; Gale, C. P.; Burley, V. J. (19 December 2013). "Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis". BMJ. 347 (dec19 2): f6879. doi:10.1136/bmj.f6879. PMC 3898422. PMID 24355537.
^ "Fats and fatty acids in human nutrition Report of an expert consultation". World Health Organization. WHO/FAO. Archived from the original on 28 December 2014. Retrieved 20 December 2014.
^ abc Willett, WC (July 2012). "Dietary fats and coronary heart disease". Journal of Internal Medicine. 272 (1): 13–24. doi:10.1111/j.1365-2796.2012.02553.x. PMID 22583051.
^ abc Chowdhury, Rajiv; Warnakula, Samantha; Kunutsor, Setor; Crowe, Francesca; Ward, Heather A.; Johnson, Laura; Franco, Oscar H.; Butterworth, Adam S.; Forouhi, Nita G.; Thompson, Simon G.; Khaw, Kay-Tee; Mozaffarian, Dariush; Danesh, John; Di Angelantonio, Emanuele (18 March 2014). "Association of Dietary, Circulating, and Supplement Fatty Acids With Coronary Risk". Annals of Internal Medicine. 160 (6): 398–406. doi:10.7326/M13-1788. PMID 24723079.
^ ab Ramsden, CE; Zamora, D; Leelarthaepin, B; Majchrzak-Hong, SF; Faurot, KR; Suchindran, CM; Ringel, A; Davis, JM; Hibbeln, JR (Feb 4, 2013). "Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis". BMJ. 346: e8707. doi:10.1136/bmj.e8707. PMC 4688426. PMID 23386268.
^ ab de Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, Uleryk E, Budylowski P, Schünemann H, Beyene J, Anand SS (Aug 12, 2015). "Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies". BMJ. 351 (h3978): h3978. doi:10.1136/bmj.h3978. PMC 4532752. PMID 26268692.
^ Hooper, L; Summerbell, CD; Thompson, R; Sills, D; Roberts, FG; Moore, HJ; Davey Smith, G (May 16, 2012). "Reduced or modified dietary fat for preventing cardiovascular disease" (PDF). Cochrane Database of Systematic Reviews. 5 (5): CD002137. doi:10.1002/14651858.CD002137.pub3. PMID 22592684.
^ Siri-Tarino Patty W; Sun Qi; Hu Frank B; Krauss Ronald M (2010). "Saturated fat, carbohydrate, and cardiovascular disease". American Journal of Clinical Nutrition. 91 (3): 502–509. doi:10.3945/ajcn.2008.26285. PMC 2824150. PMID 20089734.
^ Micha, R; Mozaffarian, D (October 2010). "Saturated fat and cardiometabolic risk factors, coronary heart disease, stroke, and diabetes: a fresh look at the evidence". Lipids. 45 (10): 893–905. doi:10.1007/s11745-010-3393-4. PMC 2950931. PMID 20354806.
^ Astrup, A; Dyerberg, J; Elwood, P; Hermansen, K; Hu, FB; Jakobsen, MU; Kok, FJ; Krauss, RM; Lecerf, JM; LeGrand, P; Nestel, P; Risérus, U; Sanders, T; Sinclair, A; Stender, S; Tholstrup, T; Willett, WC (April 2011). "The role of reducing intakes of saturated fat in the prevention of cardiovascular disease: where does the evidence stand in 2010?". The American Journal of Clinical Nutrition. 93 (4): 684–8. doi:10.3945/ajcn.110.004622. PMC 3138219. PMID 21270379.
^ Rizos, EC; Ntzani, EE; Bika, E; Kostapanos, MS; Elisaf, MS (Sep 12, 2012). "Association between omega-3 fatty acid supplementation and risk of major cardiovascular disease events: a systematic review and meta-analysis". JAMA. 308 (10): 1024–33. doi:10.1001/2012.jama.11374. PMID 22968891.
^ Abdelhamid, Asmaa S; Brown, Tracey J; Brainard, Julii S; Biswas, Priti; Thorpe, Gabrielle C; Moore, Helen J; Deane, Katherine HO; AlAbdulghafoor, Fai K; Summerbell, Carolyn D; Worthington, Helen V; Song, Fujian; Hooper, Lee (18 July 2018). "Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease". Cochrane Database of Systematic Reviews. 7: CD003177. doi:10.1002/14651858.CD003177.pub3. PMID 30019766.
^ Adler, AJ; Taylor, F; Martin, N; Gottlieb, S; Taylor, RS; Ebrahim, S (18 December 2014). "Reduced dietary salt for the prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews (12): CD009217. doi:10.1002/14651858.CD009217.pub3. PMID 25519688.
^ He, F J; MacGregor G A (2011). "Salt reduction lowers cardiovascular risk: meta-analysis of outcome trials" (PDF). The Lancet. 378 (9789): 380–382. doi:10.1016/S0140-6736(11)61174-4. PMID 21803192. Archived (PDF) from the original on 2013-12-20.
^ Paterna, S; Gaspare P; Fasullo S; Sarullo FM; Di Pasquale P (2008). "Normal-sodium diet compared with low-sodium diet in compensated congestive heart failure: is sodium an old enemy or a new friend?". Clinical Science. 114 (3): 221–230. doi:10.1042/CS20070193. PMID 17688420. Archived from the original on 2013-12-08.
^ ab Bochud, M; Marques-Vidal, P; Burnier, M; Paccaud, F (2012). "Dietary Salt Intake and Cardiovascular Disease: Summarizing the Evidence". Public Health Reviews. 33: 530–552. Archived from the original on 2013-12-21.
^ Cook, N R; et al. (2007). "Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP)". BMJ. 334 (7599): 885–8. doi:10.1136/bmj.39147.604896.55. PMC 1857760. PMID 17449506. Archived from the original on 2013-08-03.
^ Blood Pressure Lowering Treatment Trialists' Collaboration; Turnbull, F.; Neal, B.; Ninomiya, T.; Algert, C.; Arima, H.; Barzi, F.; Bulpitt, C.; Chalmers, J. (2008-05-17). "Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials". BMJ. 336 (7653): 1121–1123. doi:10.1136/bmj.39548.738368.BE. ISSN 1756-1833. PMC 2386598. PMID 18480116.
^ Blood Pressure Lowering Treatment Trialists' Collaboration; Sundström, Johan; Arima, Hisatomi; Woodward, Mark; Jackson, Rod; Karmali, Kunal; Lloyd-Jones, Donald; Baigent, Colin; Emberson, Jonathan (2014-08-16). "Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data". Lancet. 384 (9943): 591–598. doi:10.1016/S0140-6736(14)61212-5. ISSN 1474-547X. PMID 25131978.
^ Czernichow, Sébastien; Zanchetti, Alberto; Turnbull, Fiona; Barzi, Federica; Ninomiya, Toshiaru; Kengne, André-Pascal; Lambers Heerspink, Hiddo J.; Perkovic, Vlado; Huxley, Rachel (2011-01-01). "The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials". Journal of Hypertension. 29 (1): 4–16. doi:10.1097/HJH.0b013e32834000be. ISSN 1473-5598. PMID 20881867.
^ ab Turnbull, Fiona; Blood Pressure Lowering Treatment Trialists' Collaboration (2003-11-08). "Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials". Lancet (Submitted manuscript). 362 (9395): 1527–1535. doi:10.1016/s0140-6736(03)14739-3. ISSN 1474-547X. PMID 14615107.
^ Go, Alan S.; Bauman, Mary Ann; Coleman King, Sallyann M.; Fonarow, Gregg C.; Lawrence, Willie; Williams, Kim A.; Sanchez, Eduardo; American Heart Association; American College of Cardiology (2014-04-01). "An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention". Hypertension. 63 (4): 878–885. doi:10.1161/HYP.0000000000000003. ISSN 1524-4563. PMID 24243703.
^ ab Gutierrez, J; Ramirez, G; Rundek, T; Sacco, RL (Jun 25, 2012). "Statin Therapy in the Prevention of Recurrent Cardiovascular Events: A Sex-Based Meta-analysisStatin Therapy to Prevent Recurrent CV Events". Archives of Internal Medicine. 172 (12): 909–19. doi:10.1001/archinternmed.2012.2145. PMID 22732744.
^ Taylor, F; Huffman, MD; Macedo, AF; Moore, TH; Burke, M; Davey Smith, G; Ward, K; Ebrahim, S (Jan 31, 2013). "Statins for the primary prevention of cardiovascular disease" (PDF). Cochrane Database of Systematic Reviews. 1 (1): CD004816. doi:10.1002/14651858.CD004816.pub5. PMID 23440795.
^ "Statins in primary cardiovascular prevention?". Prescrire International. 27 (195): 183. July–August 2018. Retrieved 4 August 2018.
^ Downs, JR; O'Malley, PG (18 August 2015). "Management of dyslipidemia for cardiovascular disease risk reduction: synopsis of the 2014 U.S. Department of Veterans Affairs and U.S. Department of Defense clinical practice guideline". Annals of Internal Medicine. 163 (4): 291–7. doi:10.7326/m15-0840. PMID 26099117.
^ Keene, D; Price, C; Shun-Shin, MJ; Francis, DP (Jul 18, 2014). "Effect on cardiovascular risk of high density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: meta-analysis of randomised controlled trials including 117,411 patients". BMJ. 349: g4379. doi:10.1136/bmj.g4379. PMC 4103514. PMID 25038074.
^ Holman, Rury R; Sourij, Harald; Califf, Robert M (2014). "Cardiovascular outcome trials of glucose-lowering drugs or strategies in type 2 diabetes". The Lancet. 383 (9933): 2008–2017. doi:10.1016/s0140-6736(14)60794-7. PMID 24910232.
^ Control Group; Turnbull, F. M.; Abraira, C.; Anderson, R. J.; Byington, R. P.; Chalmers, J. P.; Duckworth, W. C.; Evans, G. W.; Gerstein, H. C. (2009-11-01). "Intensive glucose control and macrovascular outcomes in type 2 diabetes". Diabetologia. 52 (11): 2288–2298. doi:10.1007/s00125-009-1470-0. ISSN 1432-0428. PMID 19655124.
^ Berger, JS; Lala, A; Krantz, MJ; Baker, GS; Hiatt, WR (July 2011). "Aspirin for the prevention of cardiovascular events in patients without clinical cardiovascular disease: a meta-analysis of randomized trials". American Heart Journal. 162 (1): 115–24.e2. doi:10.1016/j.ahj.2011.04.006. PMID 21742097.
^ "Final Recommendation Statement Aspirin for the Prevention of Cardiovascular Disease: Preventive Medication". March 2009. Archived from the original on 10 January 2015. Retrieved 15 January 2015.
^ US Preventive Services Task, Force (17 March 2009). "Aspirin for the prevention of cardiovascular disease: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 150 (6): 396–404. doi:10.7326/0003-4819-150-6-200903170-00008. PMID 19293072.
^ American College of Chest Physicians; American Thoracic Society (September 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Chest Physicians and American Thoracic Society, archived from the original on 3 November 2013, retrieved 6 January 2013
^ Lee, I.-Min; Shiroma, Eric J.; Lobelo, Felipe; Puska, Pekka; Blair, Steven N.; Katzmarzyk, Peter T.; Lancet Physical Activity Series Working Group (2012-07-21). "Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy". Lancet. 380 (9838): 219–229. doi:10.1016/S0140-6736(12)61031-9. ISSN 1474-547X. PMC 3645500. PMID 22818936.
^ Hartley, Louise; Dyakova, Mariana; Holmes, Jennifer; Clarke, Aileen; Lee, Myeong Soo; Ernst, Edzard; Rees, Karen (2014-05-13). "Yoga for the primary prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews (5): CD010072. doi:10.1002/14651858.CD010072.pub2. ISSN 1469-493X. PMID 24825181.
^ Bhupathiraju, SN; Tucker, KL (Aug 17, 2011). "Coronary heart disease prevention: nutrients, foods, and dietary patterns". Clinica Chimica Acta. 412 (17–18): 1493–514. doi:10.1016/j.cca.2011.04.038. PMC 5945285. PMID 21575619.
^ Myung, SK; Ju, W; Cho, B; Oh, SW; Park, SM; Koo, BK; Park, BJ; for the Korean Meta-Analysis (KORMA) Study, Group (Jan 18, 2013). "Efficacy of vitamin and antioxidant supplements in prevention of cardiovascular disease: systematic review and meta-analysis of randomised controlled trials". BMJ. 346: f10. doi:10.1136/bmj.f10. PMC 3548618. PMID 23335472.
^ Kim, Joonseok; Choi, Jaehyoung; Kwon, Soo Young; McEvoy, John W.; Blaha, Michael J.; Blumenthal, Roger S.; Guallar, Eliseo; Zhao, Di; Michos, Erin D. (10 July 2018). "Association of Multivitamin and Mineral Supplementation and Risk of Cardiovascular Disease". Circulation: Cardiovascular Quality and Outcomes. 11 (7): e004224. doi:10.1161/CIRCOUTCOMES.117.004224. PMID 29991644.
^ Fortmann, SP; Burda, BU; Senger, CA; Lin, JS; Whitlock, EP (Nov 12, 2013). "Vitamin and Mineral Supplements in the Primary Prevention of Cardiovascular Disease and Cancer: An Updated Systematic Evidence Review for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 159 (12): 824–34. doi:10.7326/0003-4819-159-12-201312170-00729. PMID 24217421.
^ Bruckert, E; Labreuche, J; Amarenco, P (June 2010). "Meta-analysis of the effect of nicotinic acid alone or in combination on cardiovascular events and atherosclerosis". Atherosclerosis. 210 (2): 353–61. doi:10.1016/j.atherosclerosis.2009.12.023. PMID 20079494.
^ Lavigne, PM; Karas, RH (Jan 29, 2013). "The current state of niacin in cardiovascular disease prevention: a systematic review and meta-regression". Journal of the American College of Cardiology. 61 (4): 440–6. doi:10.1016/j.jacc.2012.10.030. PMID 23265337.
^ Jee SH, Miller ER, Guallar E, et al. (2002). "The effect of magnesium supplementation on blood pressure: a meta-analysis of randomized clinical trials". Am J Hypertens. 15 (8): 691–696. doi:10.1016/S0895-7061(02)02964-3. PMID 12160191.
^ Zipes DP, Camm AJ, Borggrefe M, et al. (2012). "ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation. 114 (10): e385–e484. doi:10.1161/CIRCULATIONAHA.106.178233. PMID 16935995.
^ Kwak, SM; Myung, SK; Lee, YJ; Seo, HG; for the Korean Meta-analysis Study, Group (Apr 9, 2012). "Efficacy of Omega-3 Fatty Acid Supplements (Eicosapentaenoic Acid and Docosahexaenoic Acid) in the Secondary Prevention of Cardiovascular Disease: A Meta-analysis of Randomized, Double-blind, Placebo-Controlled Trials". Archives of Internal Medicine. 172 (9): 686–94. doi:10.1001/archinternmed.2012.262. PMID 22493407.
^ Clar, Christine; Oseni, Zainab; Flowers, Nadine; Keshtkar-Jahromi, Maryam; Rees, Karen (2015-05-05). "Influenza vaccines for preventing cardiovascular disease". The Cochrane Database of Systematic Reviews (5): CD005050. doi:10.1002/14651858.CD005050.pub3. ISSN 1469-493X. PMID 25940444.
^ Shanthi, Mendis; Pekka, Puska; Bo, Norrving (2011-01-01). Global atlas on cardiovascular disease prevention and control. World Health Organization. ISBN 9789241564373. OCLC 796362754.
^ Indian Heart Association Why South Asians Facts Web. 29 April 2015. <"Overview". Archived from the original on 2015-05-18. Retrieved 2015-05-08.>
^ Thompson, Randall C; Allam, Adel H; Lombardi, Guido P; Wann, L Samuel; Sutherland, M Linda; Sutherland, James D; Soliman, Muhammad Al-Tohamy; Frohlich, Bruno; Mininberg, David T (2013). "Atherosclerosis across 4000 years of human history: the Horus study of four ancient populations". The Lancet. 381 (9873): 1211–1222. doi:10.1016/s0140-6736(13)60598-x. PMID 23489753.
^ Alberti, Fay Bound (2013-05-01). "John Hunter's Heart". The Bulletin of the Royal College of Surgeons of England. 95 (5): 168–169. doi:10.1308/003588413X13643054409261. ISSN 1473-6357.
^ Ruparelia, Neil; Chai, Joshua T.; Fisher, Edward A.; Choudhury, Robin P. (2016). "Inflammatory processes in cardiovascular disease: a route to targeted therapies". Nature Reviews Cardiology. 14 (3): 133–144. doi:10.1038/nrcardio.2016.185. PMC 5525550. PMID 27905474.
^ Tang, W. H. Wilson; Hazen, Stanley L. (2017-01-17). "Atherosclerosis in 2016: Advances in new therapeutic targets for atherosclerosis". Nature Reviews Cardiology. 14 (2): 71–72. doi:10.1038/nrcardio.2016.216. ISSN 1759-5010. PMC 5880294. PMID 28094270.
^ Swerdlow, Daniel I.; Humphries, Steve E. (2017-02-01). "Genetics of CHD in 2016: Common and rare genetic variants and risk of CHD". Nature Reviews Cardiology. 14 (2): 73–74. doi:10.1038/nrcardio.2016.209. ISSN 1759-5010. PMID 28054577.
External links
| Classification | D
|
|---|
Cardiovascular disease at Curlie- European Guidelines on cardiovascular disease prevention in clinical practice (version 2012)
Heart Disease MedicineNet Slides, photos, descriptions